You’ve been redirected from preventepidemics.org.
Prevent Epidemics is part of resolvetosavelives.org.
Prevent Epidemics Resource Library
Find guidance, case studies, advocacy tools and more
You’ve been redirected. LINKScommunity.org is now part of resolvetosavelives.org.
Filter by:
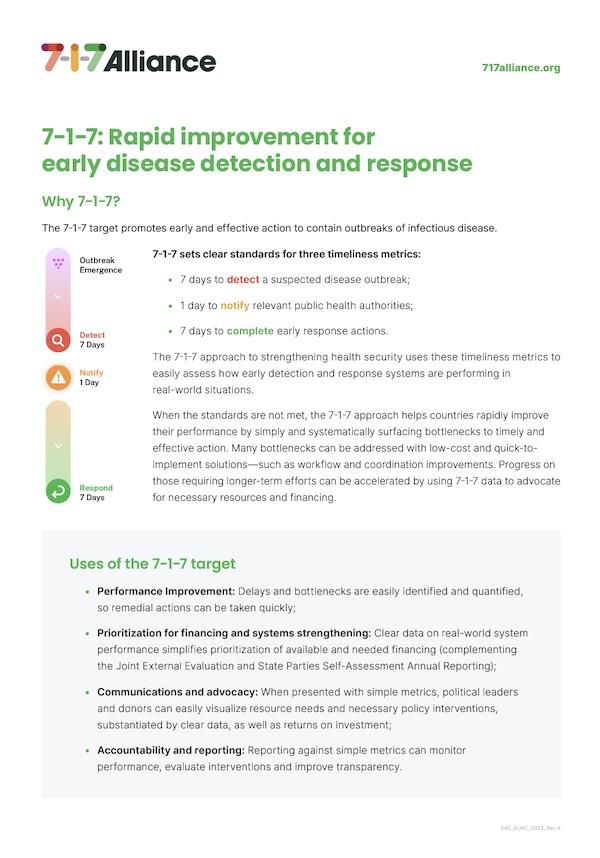
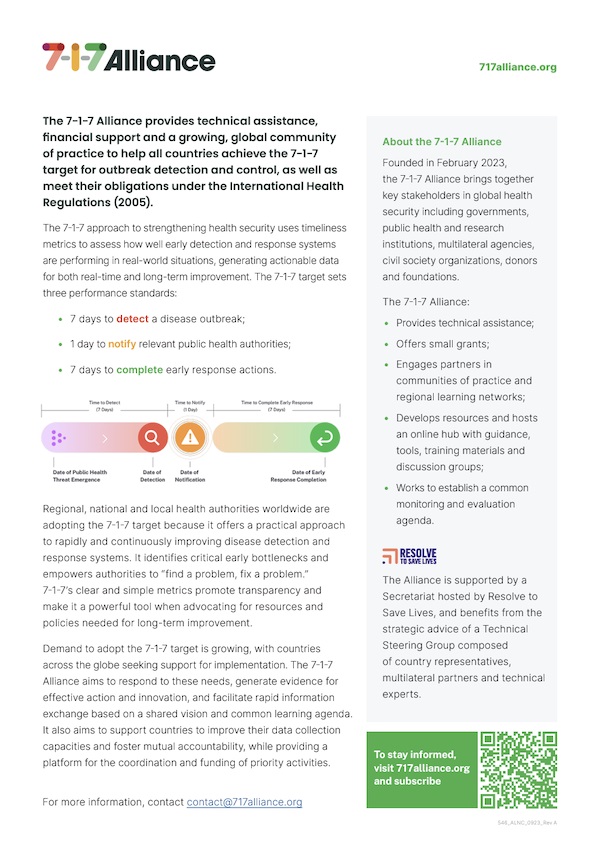
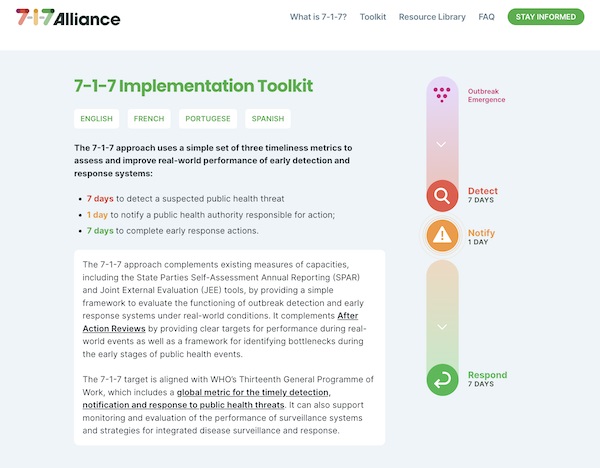
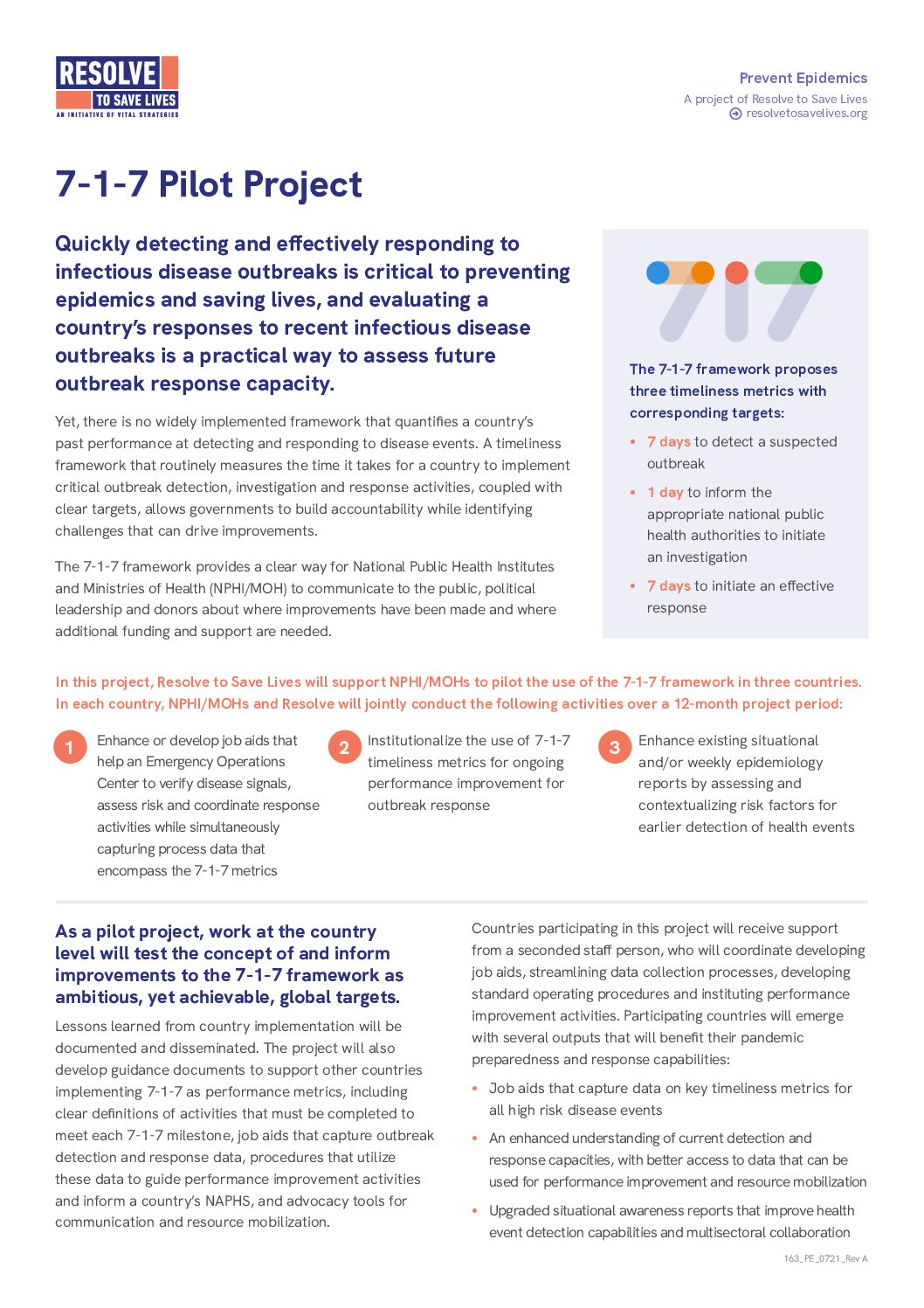
Introductory brief on the 7-1-7 target, its uses, and how it complements existing tools and assessments.
In a perspective piece published in Frontiers in Sustainable Cities, Resolve to Save Lives and partners outline ten key themes for strengthening health security in urban environments. Given cities’ unique vulnerabilities to infectious diseases, the paper highlights areas such as community partnerships, governance and financing, risk communication and resilient infrastructure as critical for epidemic preparedness. By intentionally advancing these themes, cities can better prevent, detect, respond to and recover from health threats—offering a roadmap for enhancing public health resilience in urban settings worldwide.
In a study published in Health Security, Resolve to Save Lives and partners introduce a tool for assessing subnational health security in Nigeria that evaluates state-level capacities under the International Health Regulations (2005) (IHR). With input from public health leaders and legal experts, the team used a legislative evaluation to determine feasible IHR activities within state legal frameworks to inform the tool, which was then piloted in Kano, Enugu and Kebbi states. Using 35 indicators across 14 technical areas, the tool identifies gaps in capacities and opportunities for improvement planning at the subnational level. This approach offers a model for strengthening preparedness in federated systems and geographically diverse countries.
Can 7-1-7 help household contacts of tuberculosis patients get started on preventive therapy? In the International Journal of Tuberculosis and Lung Disease, our colleagues at International Union Against Tuberculosis and Lung Disease used a mixed-methods approach to assess the feasibility of the timeliness metric in the private sector in Chennai, India. Among 263 index patients, 90% had their household contacts (HHCs) line-listed within 7 days. Screening outcomes for 48% of the 556 were achieved in HHCs within 1 day, and 57% began TPT or received a treatment decision within 7 days. 24% of screened HHCs started TPT during the ‘7-1-7’ period, compared to 16% in historical controls. Barriers included HHC reluctance to be evaluated, private providers’ refusal to prescribe TPT, and reliance on facility-based screening instead of home visits. Overall, the introduction of 7-1-7 can effectively enhance HHC screening and management.
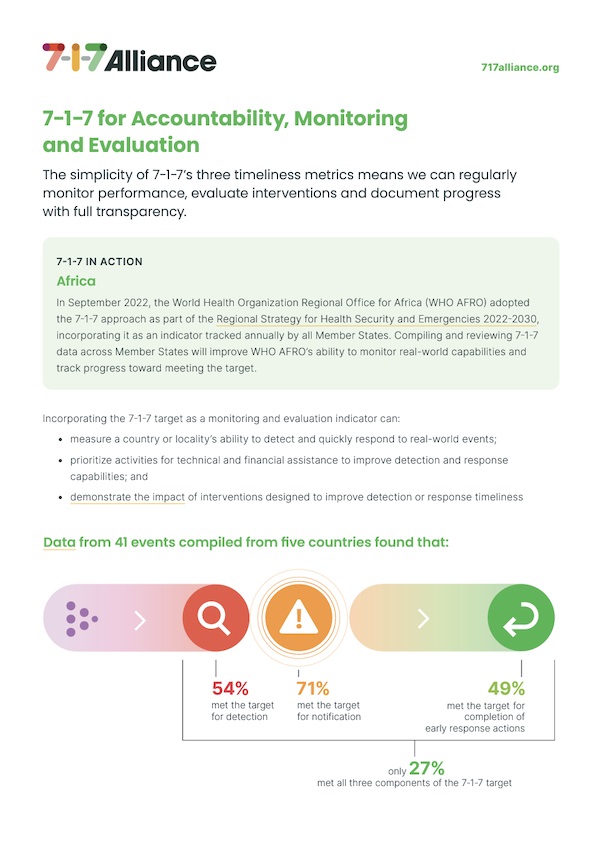
The simplicity of 7-1-7’s timeliness metrics helps monitor performance, evaluate interventions and document progress with full transparency.
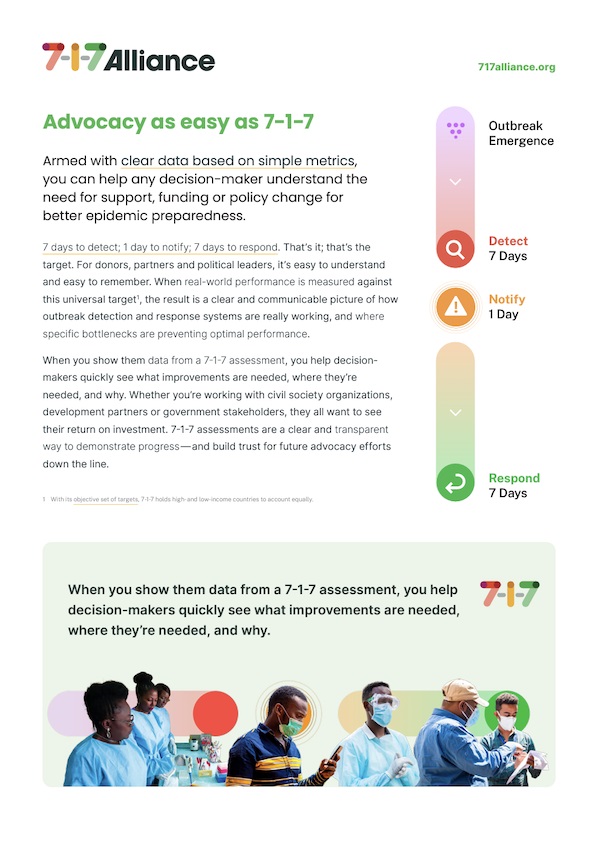
Clear data based on simple metrics can help any decision-maker understand the need for support, funding or policy change for better epidemic preparedness.
By incorporating 7-1-7 into existing workflows, we can make every outbreak an opportunity to improve how we detect and respond to infectious disease threats.
Overview of the 7-1-7 evidence base.
Introductory brief on the7-1-7 Alliance, the 7-1-7 target, and the Alliance missions.
Step-by-step guidance and tools to start putting 7-1-7 to work, in one place.
Dossier d’information sur la protection du personnel de santé pendant les épidémies.
An overview of how rapid outbreak financing are crucial to preventing epidemics.
An overview of program management for epidemic preparedness and how to strengthen health security through shared learning and peer exchange.
A brief from PERC’s 24,000-person survey conducted in 18 African Union (AU) Member States in August 2020 to assess disruptions to essential health services brought on by COVID-19.
A brief from PERC’s 24,000-person survey conducted in 18 African Union (AU) Member States in August 2020 to assess the household-level economic burden of COVID-19.
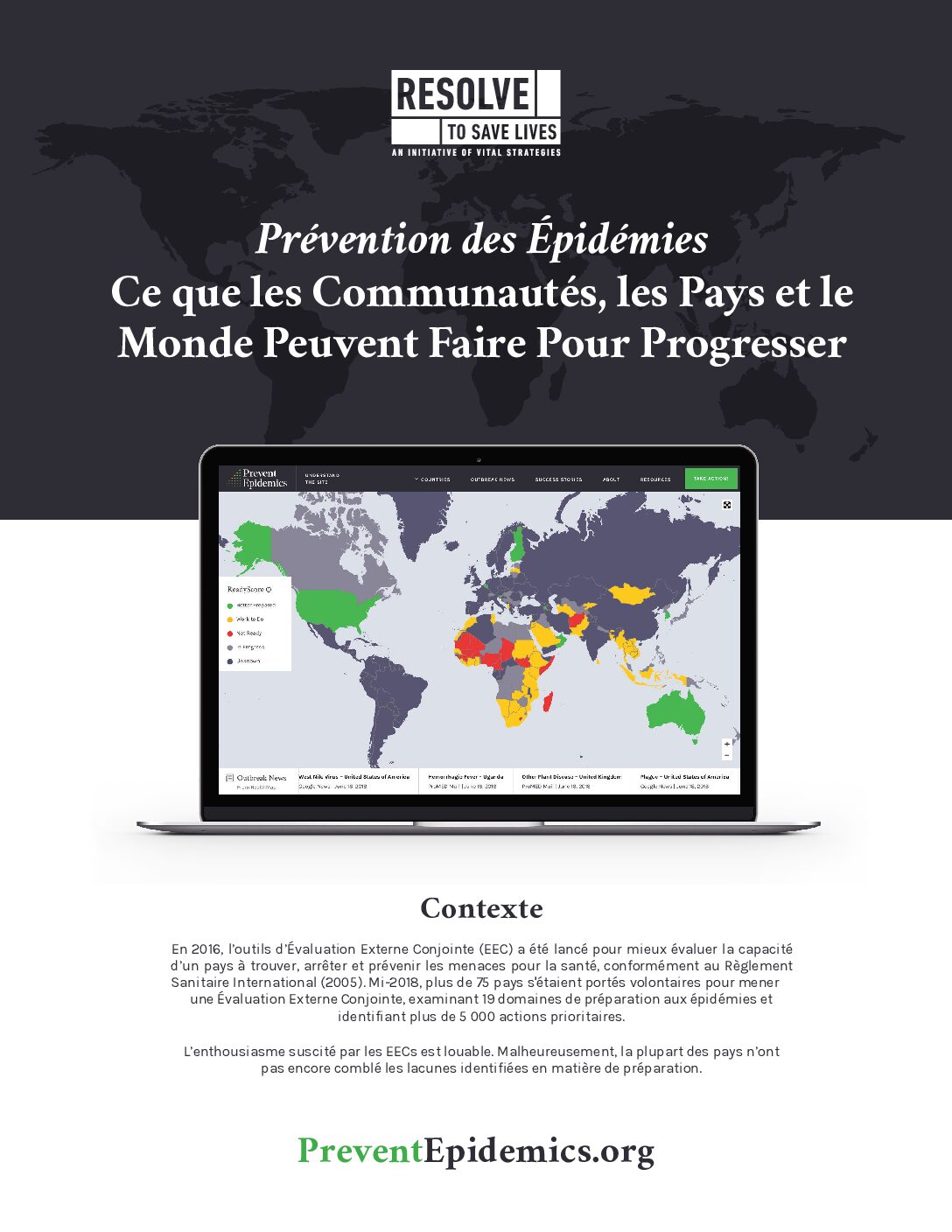
Fiche d’information sur les actions clés pour faire progresser la prévention des épidémies.
Fiche d’information sur les actions clés pour prévenir les épidémies.
Ensiegnements et recommandations tirés des travaux menés par Resolve to Save Lives et l’Association internationale des instituts nationaux de santé publique conjointement avec des partenaires dans de nombreux pays.
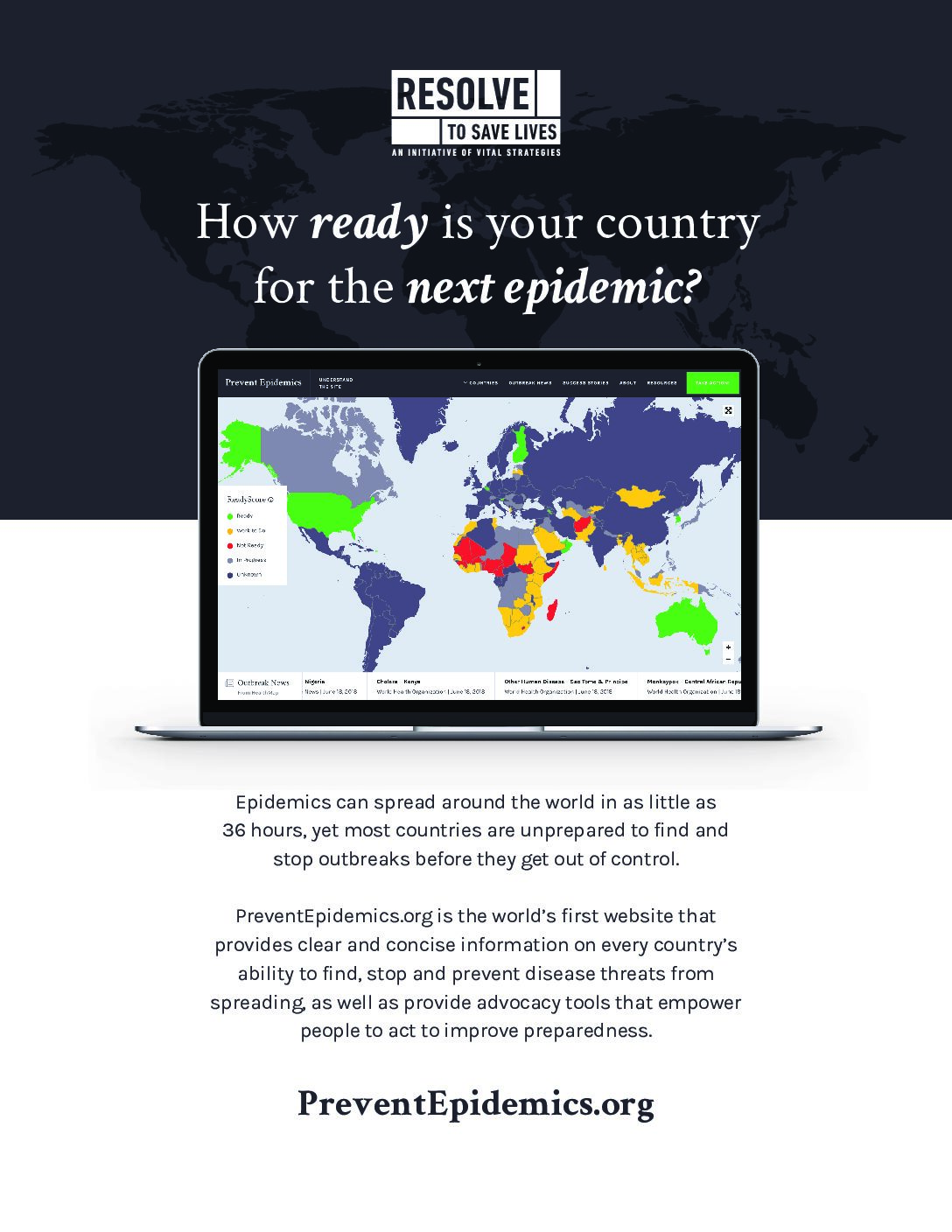
Guidance on identifying your country’s readiness score for country-level epidemic preparedness.
A letter to US congressional leaders urging the extension of paid sick leave benefits during the COVID-19 pandemic.
An overview of the process of developing the 2024 National Action Plan for Health Security Annual Operational Plan in Nigeria.
“An overview of how the National Action Plan for Health Security (NAPHS) Tracker enables data-informed decision-making to streamline
NAPHS management and financing.”
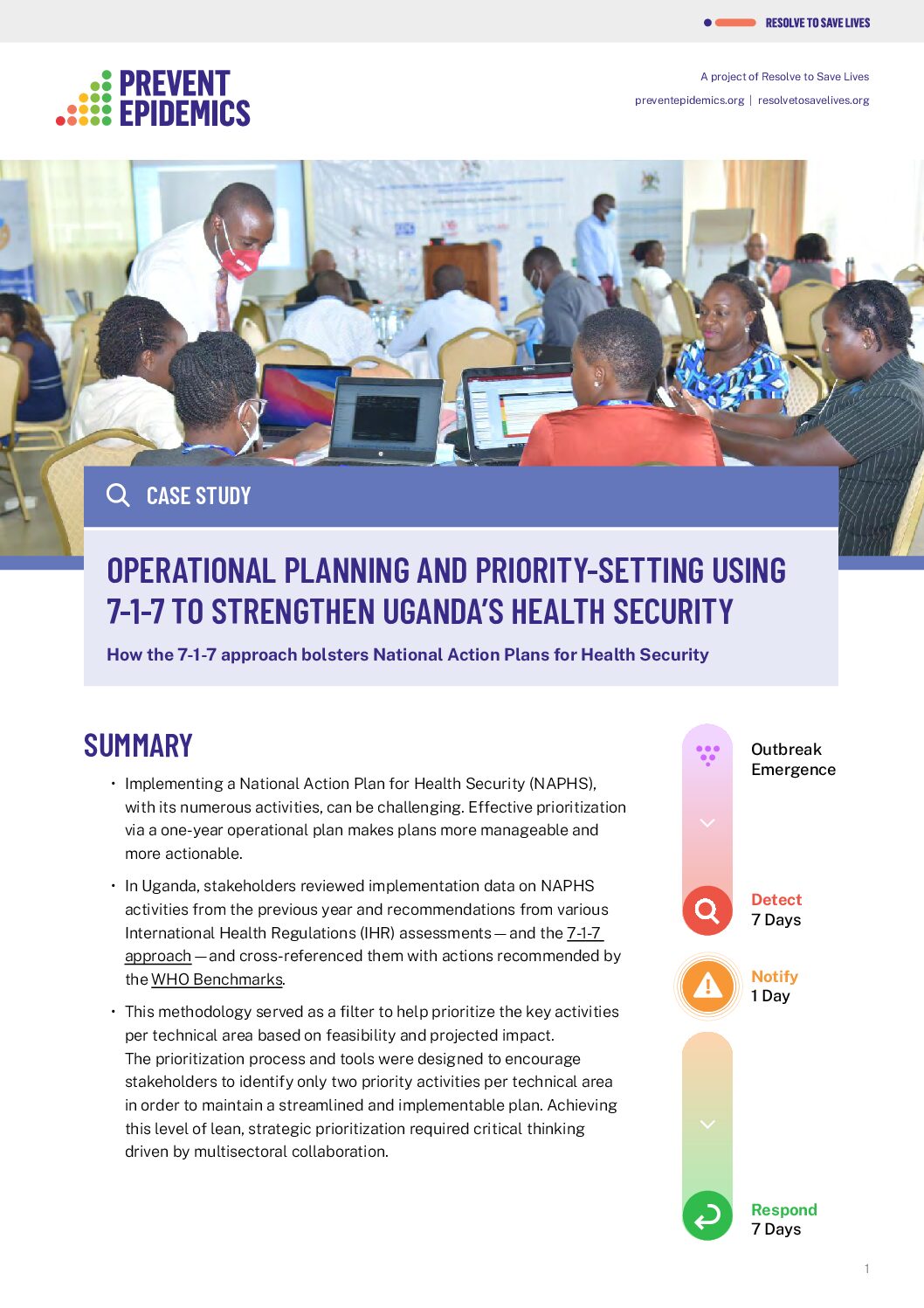
A case study on how the 7-1-7 approach bolstered Uganda’s National Action Plan for Health Security (NAPHS).
This document outlines the International Health Regulations and the core capacities countries must develop to detect, prevent, and respond to public health threats, including infectious diseases.
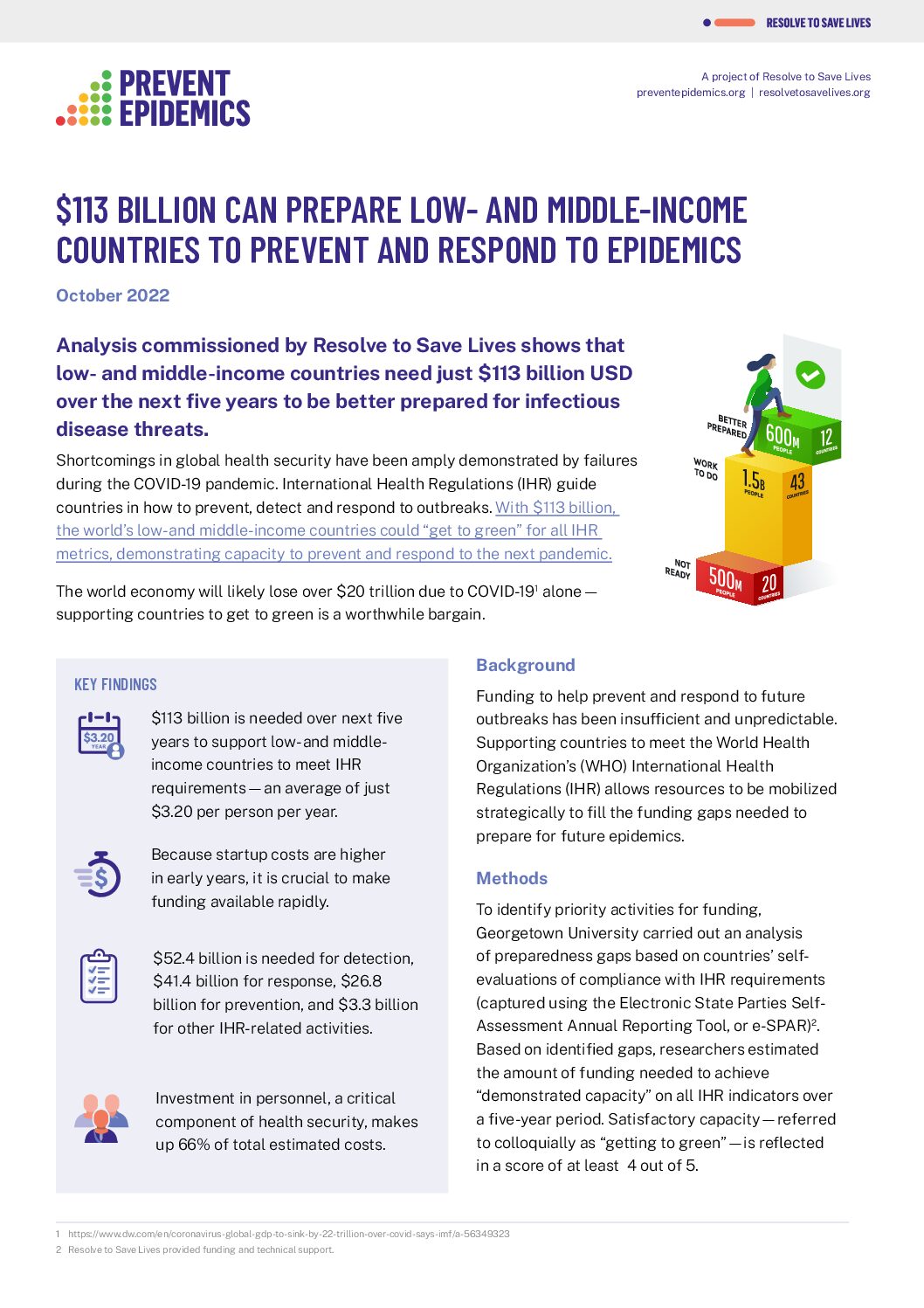
Analysis commissioned by Resolve to Save Lives shows that low- and middle-income countries need just $113 billion USD over the next five years to be better prepared for infectious disease threats.
Practical guidance on how to effectively conduct a Training of Trainers (ToT). It covers essential tips and best practices for facilitating interactive, engaging, and impactful training, including preparation strategies, fostering participant engagement, and ensuring knowledge transfer.
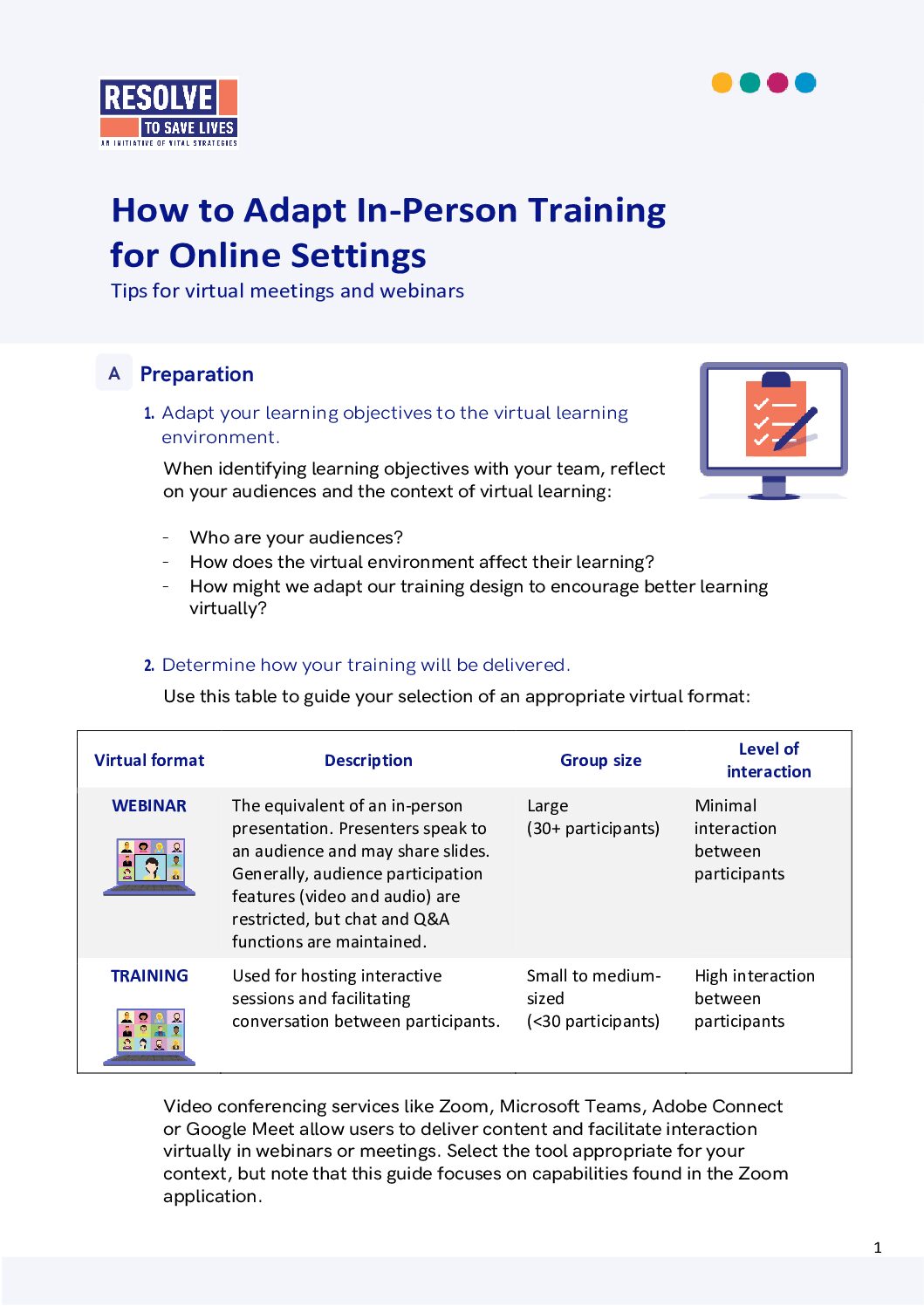
Tips and tools for facilitating online meetings, trainings and workshops.
Guide pour la mise en place d’une communauté virtuelle de pratique.
Practical guidance on how to conduct a community of practice (CoP) virtually.
Tips and tools for facilitating trainings online.
A letter to US Congress advocating for investment in health defense to prevent, detect, and respond to future outbreaks.
Référentiel pour les campagnes de plaidoyer stratégiques.
Strengthening national health security with multidisciplinary teams dedicated to epidemic preparedness.
A guide designed to help civil society organizations plan and conduct effective advocacy campaigns that will result in the adoption and implementation of strong effective public health policies.
A guide designed to help civil society organizations plan public health media advocacy through a media advocacy campaign.
A guide designed to help civil society organizations plan a strategic policy advocacy campaign with specific details on how to conclude the campaign.
Référentiel pour les campagnes de plaidoyer stratégiques.
Référentiel pour les campagnes de plaidoyer stratégiques.
Fiche d’information sur l’évalution externe conjointe (EEC).
Fiche d’information sur le Règlement sanitaire international (RSI).
A case study on fast-tracking funding for epidemic preparedness in the Democratic Republic of Congo .
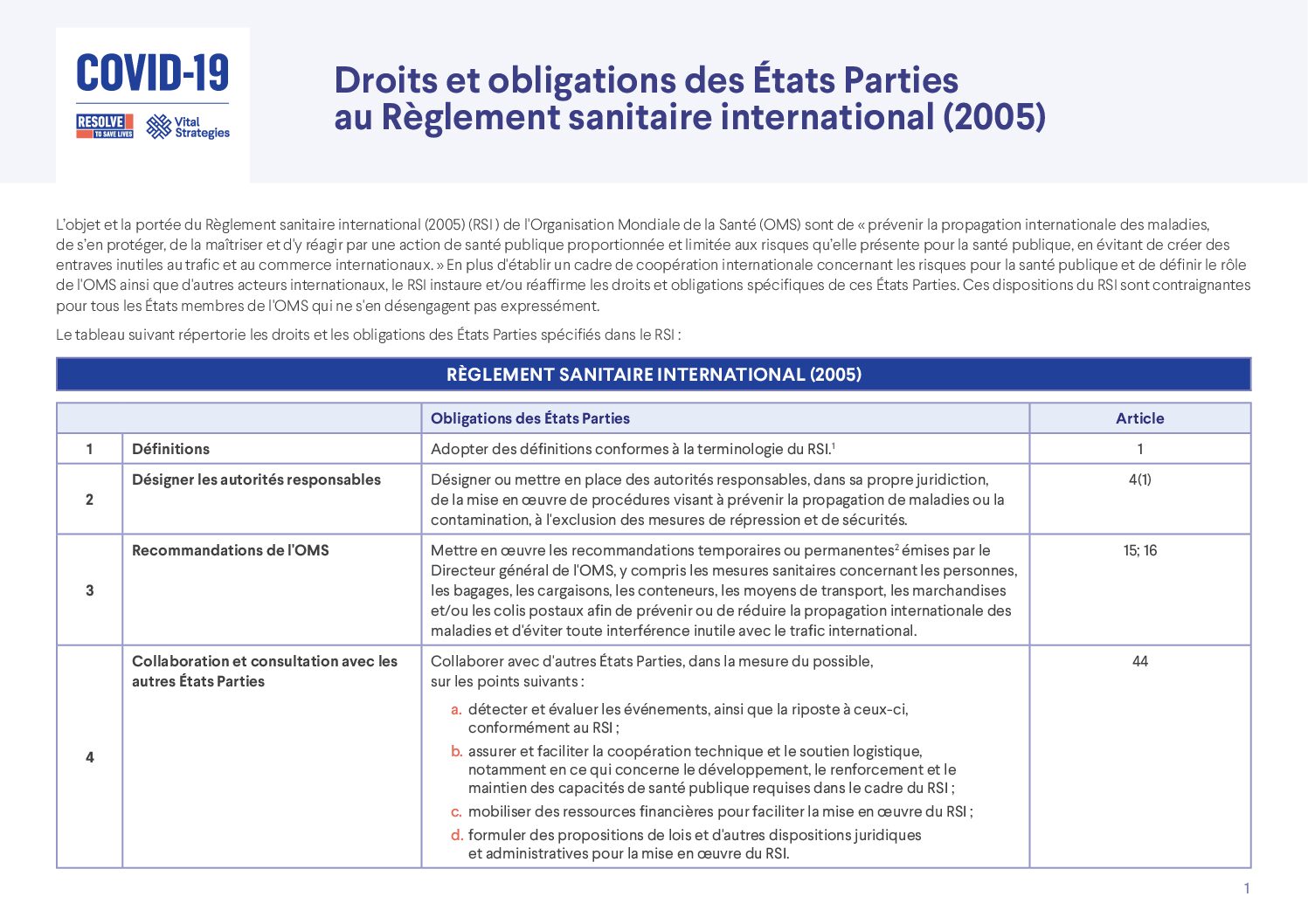
Synthèse des principaux droits et obligations des états parties au Règlement sanitaire international (2005).
Conseils et bonnes pratiques pour animer enligne des réunions, des formations et des ateliers.
Conseils et bonnes pratiques pour animer une formation de formateur.
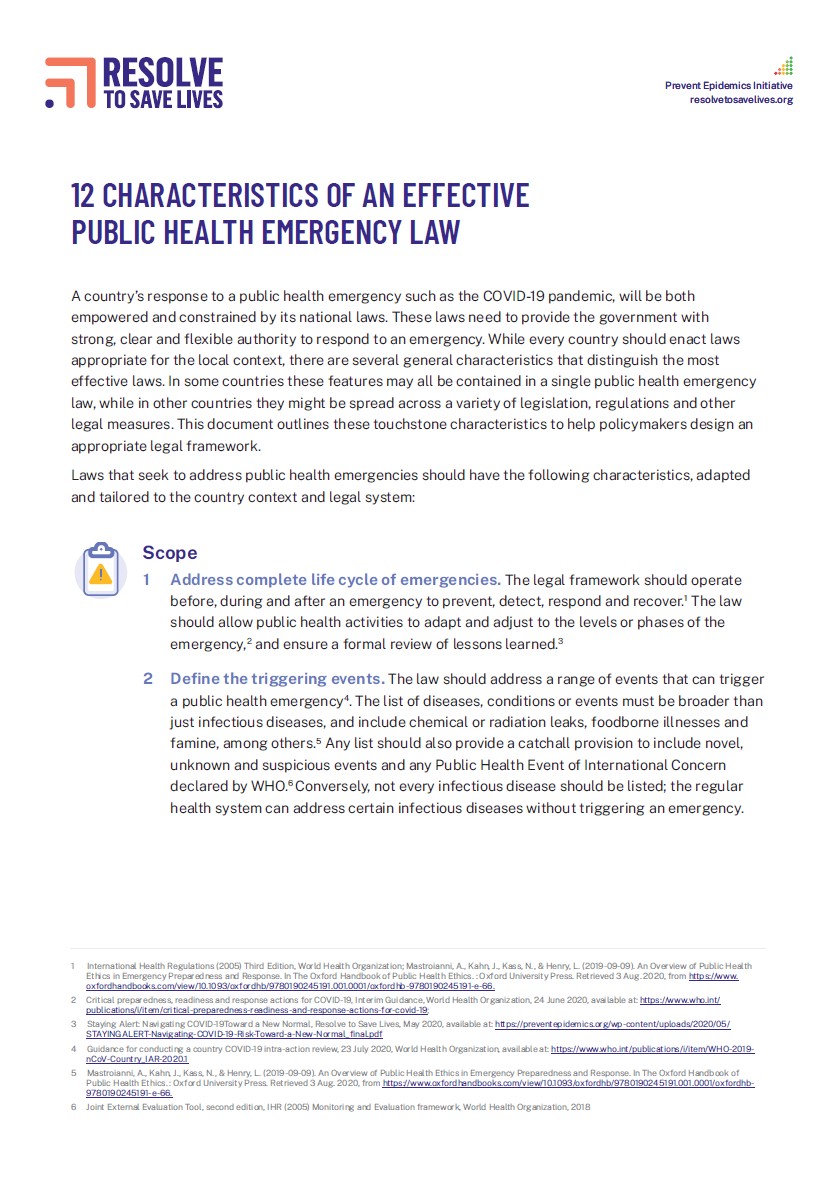
An outline of 12 characteristics that make a public health law effective, to help policymakers design appropriate legal framework.
Practical guidance to implement rapid mortality surveillance (RMS) and measure excess mortality in the context of the COVID-19 pandemic.
Practical guidance on using existing data from respiratory disease surveillance systems and hospital-based routine data systems to supplement COVID-19 surveillance and inform response activities.
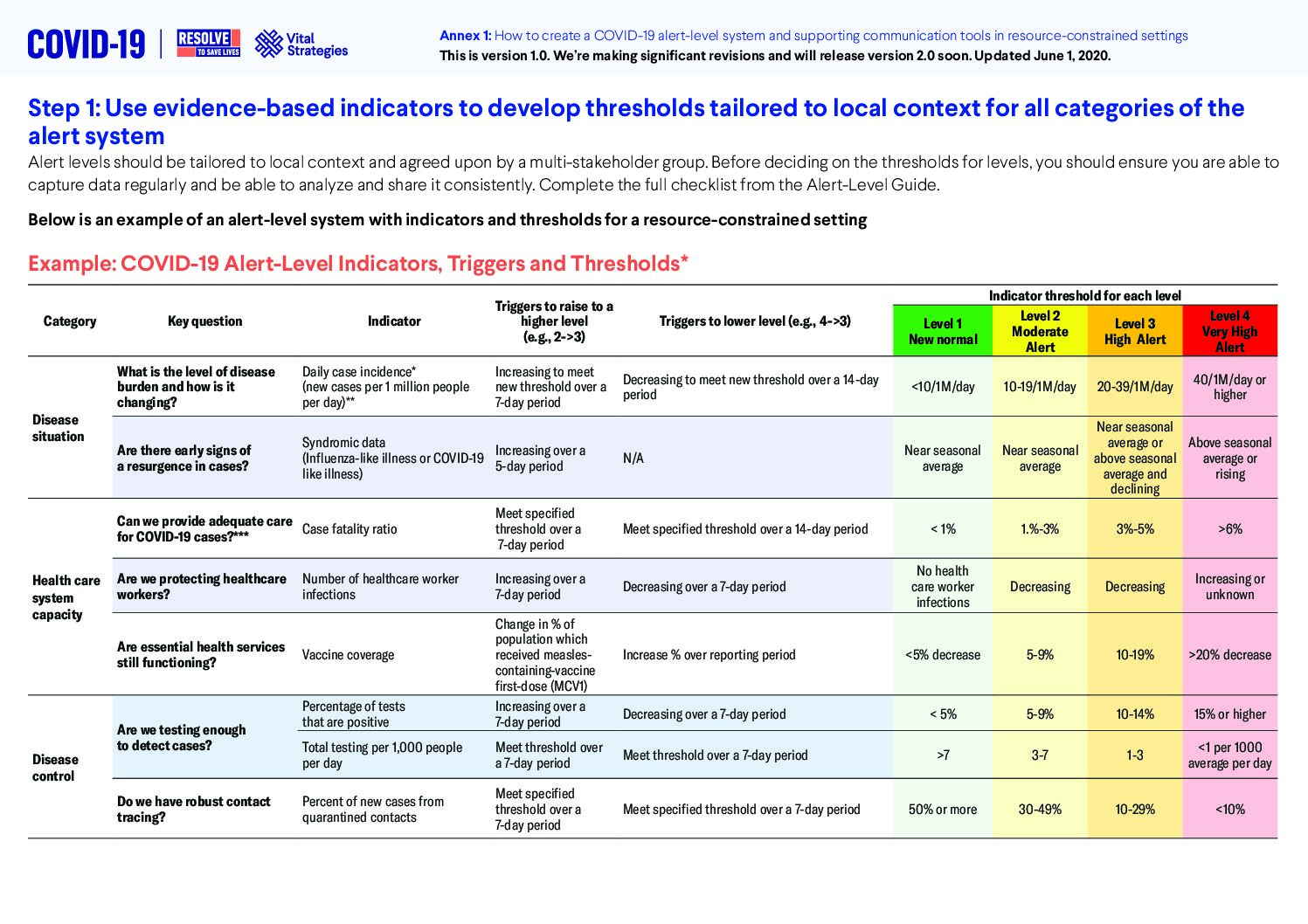
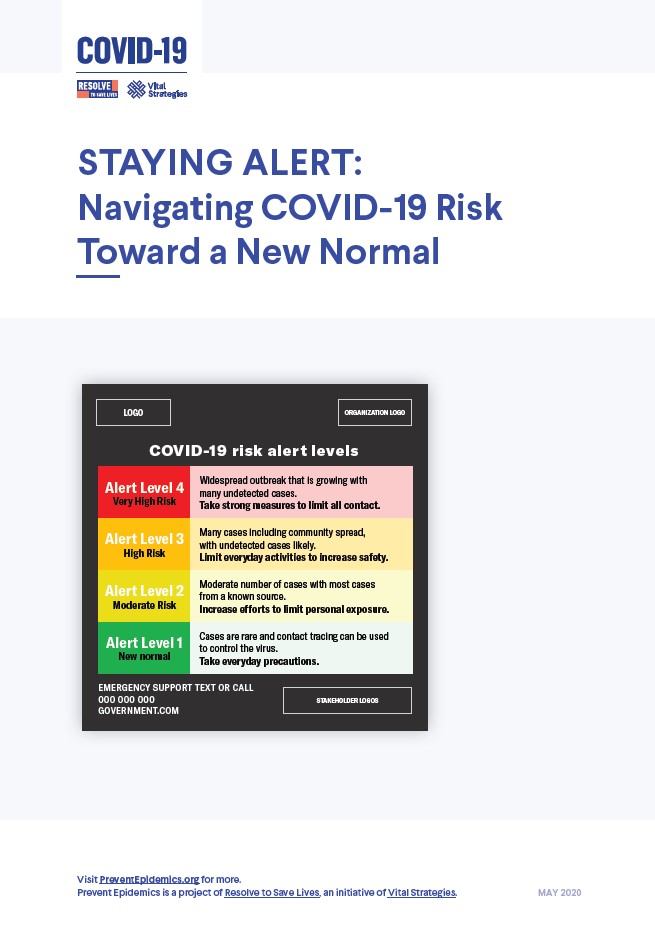
Step-by-step guidance on creating an alert-level system.
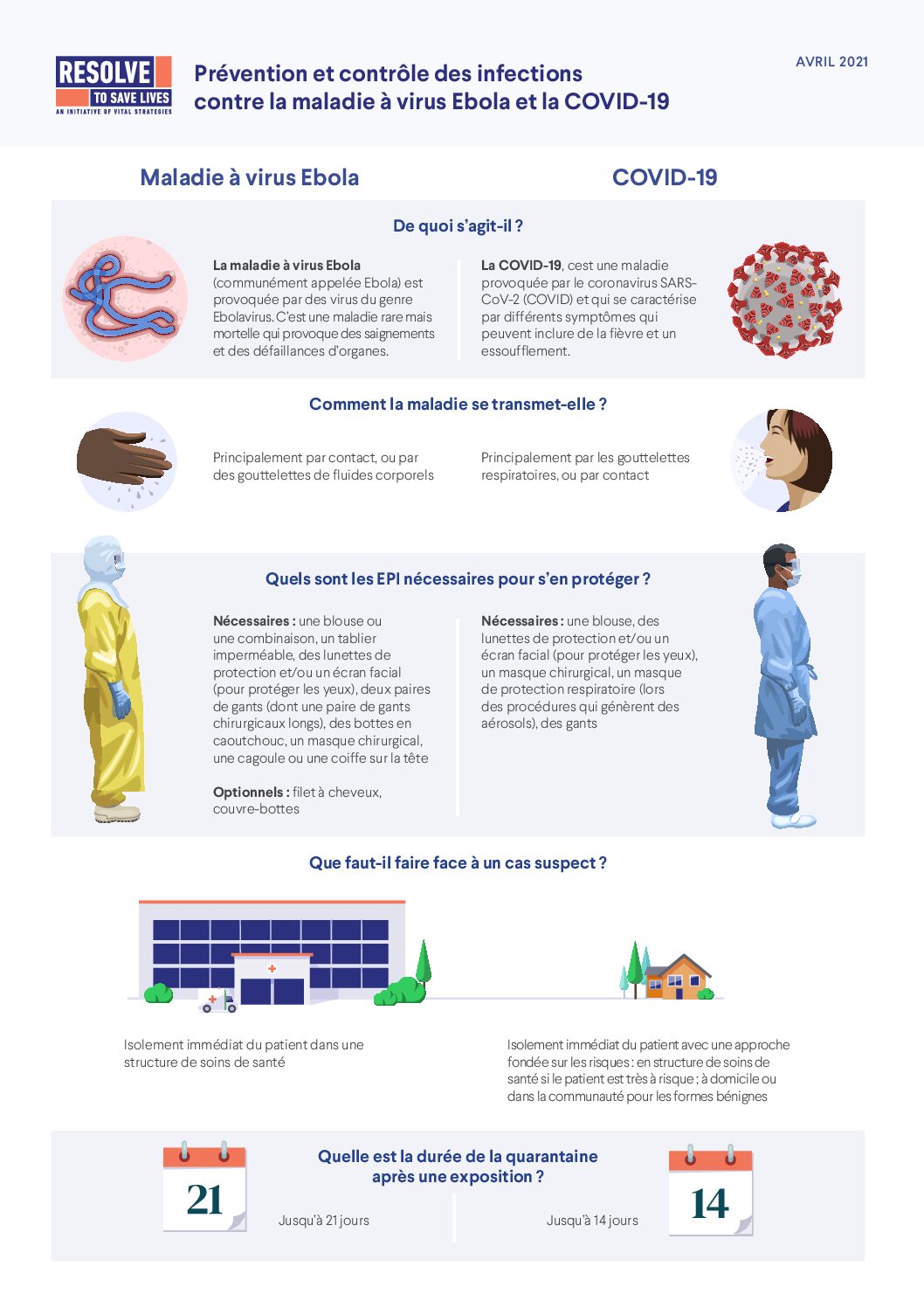
Fiche d’information sur la prévention et le contrôle des infections contre la maladie à virus Ebola et la COVID-19.
This infographic outlines key infection prevention and control measures for Ebola Virus Disease (EVD) and COVID-19, focusing on practices like hand hygiene, the proper use of personal protective equipment (PPE), safe patient handling, and waste management.
A guide designed to help civil society organizations plan a strategic policy advocacy campaign with specific details on how to talk with policy-makers.
A how-to guide designed to help civil society organizations plan a strategic policy advocacy campaign.
A toolkit designed to help civil society organizations plan a strategic policy advocacy campaign with specific details on how to coordinate strong partnerships.
A guide designed to help civil society organizations plan public health media advocacy through a media advocacy campaign.
A toolkit designed to help civil society organizations plan a strategic policy advocacy campaign.
An overview of considerations for the development of a national institute of public health for countries to utilize in their planning.
An overview of Resolve to Save Lives’ 2020 awareness campaign to highlight COVID long-haulers’ experience and urge vaccine uptake.
Fiche d’information sur le renforcement de la préparation aux épidémies au niveau national.
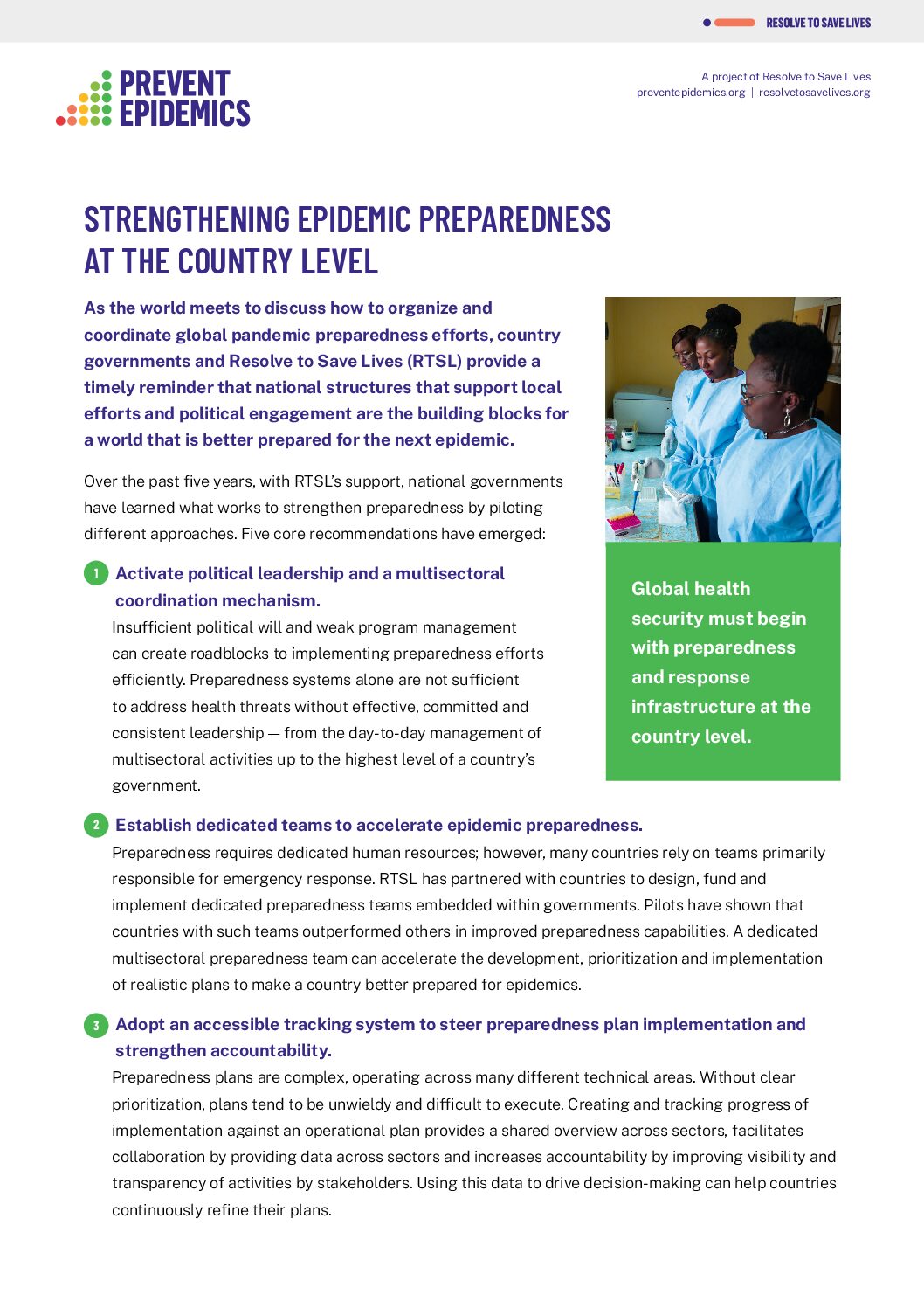
Five core recommendations from national governments that have learned what works to strengthen preparedness by piloting different approaches.
An issue brief outlining recommendations on adapting and strengthening global health so that it is fit-for-purpose for the next health threat.
Dossier d’information sur le renforcement de la préparation aux épidémies au niveau national.
A fact sheet providing an overview of the IHR with FAQ’s.
Questions fréquement posées sur le programme PMEP (Gestion des programmes pour la préparation aux épidémies).
A FAQ document on program management for epidemic preparedness.
An overview of program management and epidemic preparedness, a leadership and management program that enables teams to accelerate epidemic preparedness in their countries through thoughtful peer exchange and practical learning.
Dossier d’information sur le programme PMEP (Gestion des programmes pour la préparation aux épidémies).
The 7-1-7 framework helps countries strengthen their outbreak detection and response by setting clear targets: 7 days to detect a suspected outbreak, 1 day to inform public health authorities, and 7 days to initiate a response. This pilot project tested the framework in three countries to improve pandemic preparedness and guide performance improvements.
Fiche d’information sur les messages clés de ce qui a changé dans le pratiques de PCI qu’il est recommandé d’appliquer lors des épidémies actuelles et à venir.
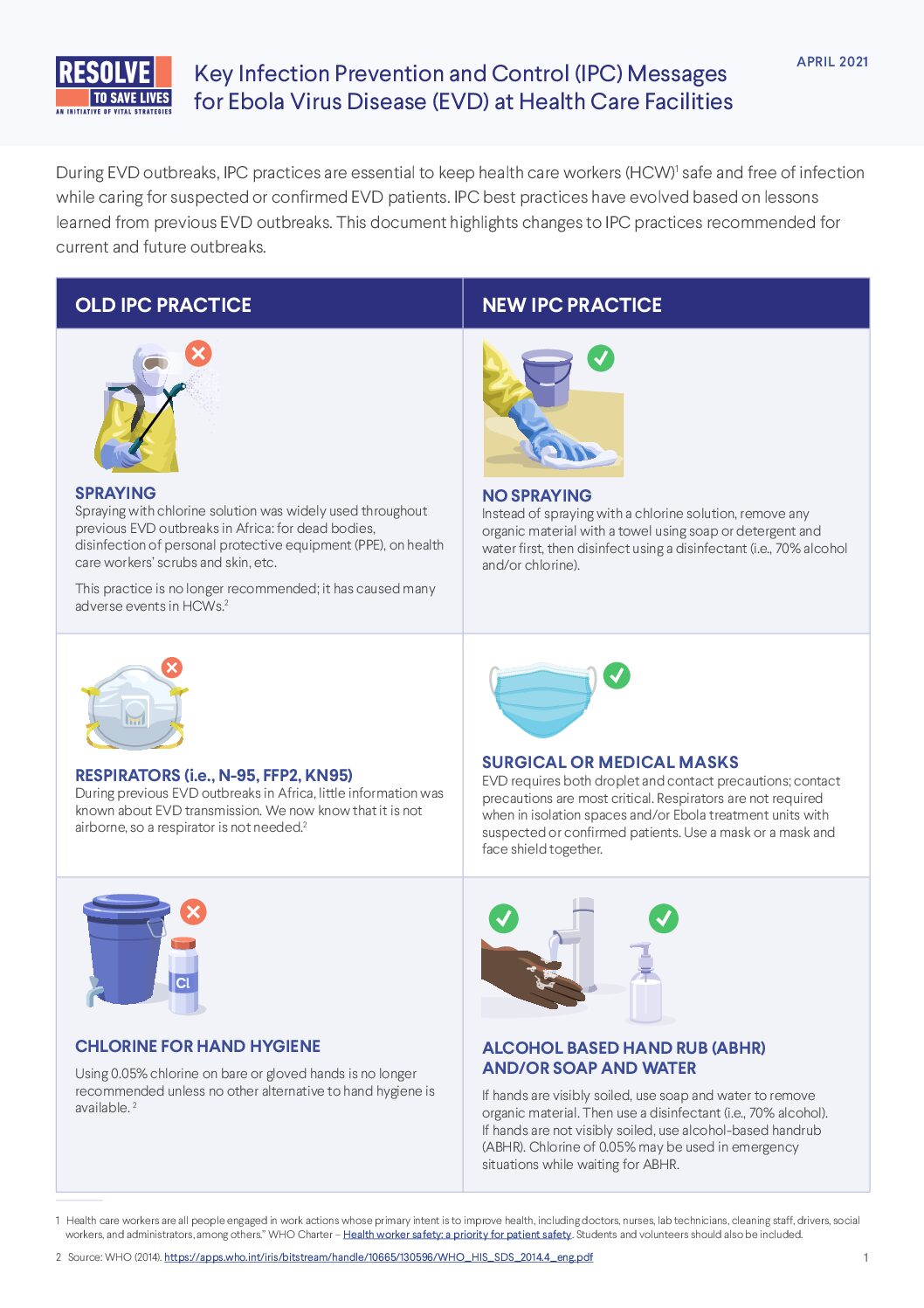
An overview of changes to infection, prevention and control (IPC) practices recommended for Ebola Virus Disease (EVD) outbreaks.
An overview of the International Health Regulations.
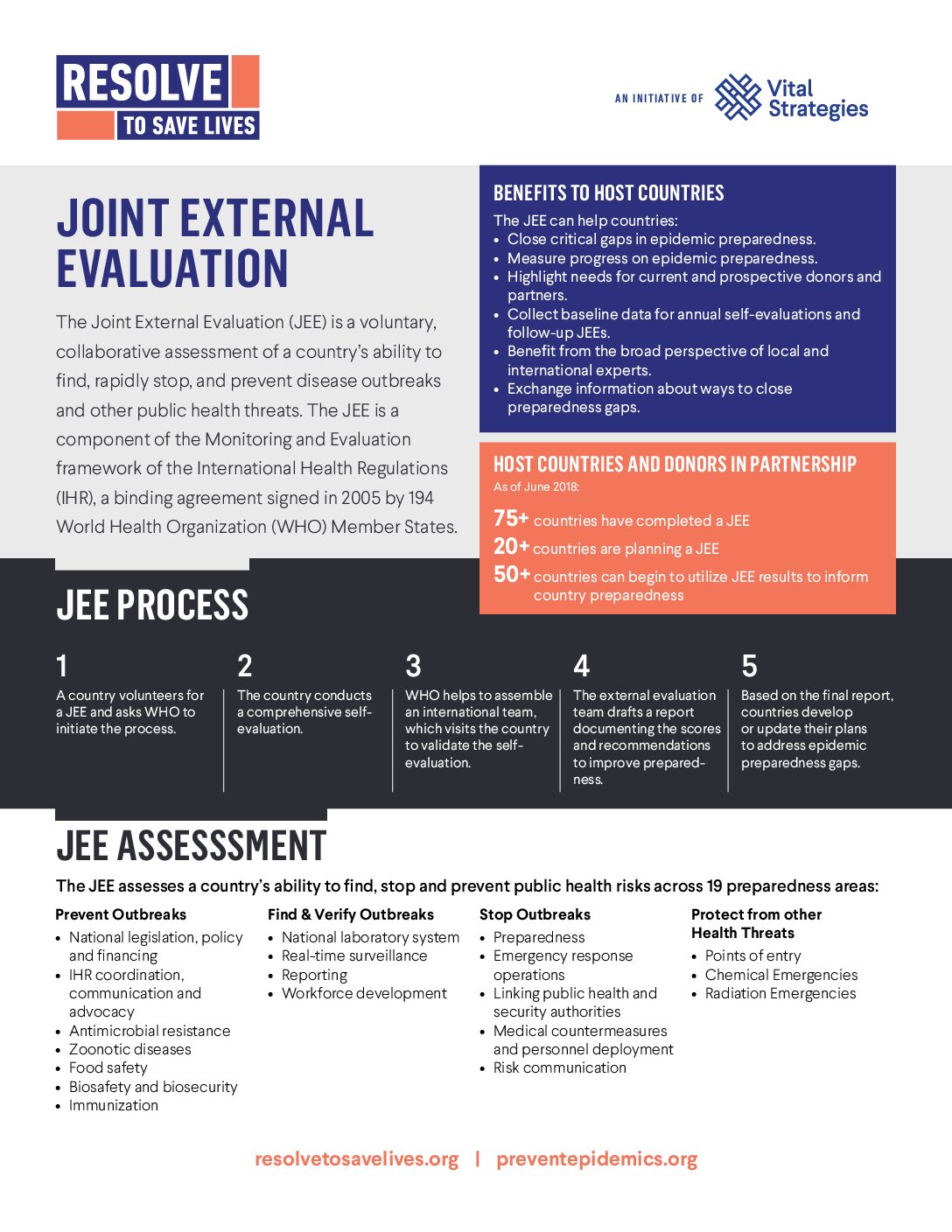
An overview of the Joint External Evaluation (JEE), a voluntary, collaborative assessment of a country’s ability to find, rapidly stop and prevent disease outbreaks and other public health threats.
A step- by-step framework to use in analyzing and improving their systems of epidemic control. This outlines targets for key completeness measures and time intervals between activities, based on mathematical models of case investigation and contact tracing, to effectively reduce COVID-19 transmission.
This document highlights the need to reduce noncommunicable disease (NCD) risk factors—such as poor nutrition, tobacco, alcohol use, and air pollution—in order to protect populations from severe COVID-19 outcomes and future pandemics. It recommends evidence-based policies, like trans fat elimination and tobacco control, to build resilience and promote healthier, longer lives.
How do local governments contribute to pandemic response? For PLOS Global Public Health, Resolve to Save Lives collaborated with colleagues at Center for Global Health Science & Security and Vital Strategies to assess government responsibilities, the timeline of response activities, challenges faced during the COVID-19 pandemic among members of the Partnership for Healthy Cities. Among the 25 participating cities, national authorities primarily led pandemic activities but local governments were crucial in risk communication and community coordination. Most activities occurred after COVID-19 confirmation, highlighting challenges in proactive preparedness; nearly all local authorities expressed a desire for greater involvement in future pandemic preparedness and response.
The Smithsonian exhibition, Outbreak: Epidemics in a Connected World, shows that the world cannot afford to wait for the next epidemic—we must act on the information that we have now to end preventable outbreaks. Writing for the Lancet, Resolve to Save Lives reflects on the impact of epidemics over the past century, from Nipah virus to HIV and Ebola. It underscores the importance of coordinated global efforts in epidemic preparedness, emphasizing the lessons learned from previous outbreaks. Despite progress, significant gaps remain in disease surveillance, community engagement, and health care capacity. A safer future for all will require ongoing education, collaboration, and a global commitment to addressing vulnerabilities.
In a study published in the International Journal of Tuberculosis and Lung Disease, our colleagues at the International Union Against Tuberculosis and Lung Disease and the Respiratory Society of Kenya evaluated the feasibility of implementing a “7-1-7” timeliness metric for screening and initiating TB preventive therapy (TPT) among household contacts (HHCs) of index patients with tuberculosis (TB) in Kiambu County, Kenya. Over six months in 12 health facilities, 95% of 508 index patients had their HHCs line-listed within 7 days, and 68% of 1,115 HHCs were screened for TB within one day. Only 62% of eligible HHCs initiated TPT within 7 days, compared with 58% in a historical cohort. Main barriers to TPT uptake included HHCs not presenting for treatment or being unwilling to initiate TPT, and drug shortages. Health care workers reported that a timeliness metric was valuable for streamlining management and proposed “3-5-7” as an alternative.
In a commentary for BMJ Global Health, Resolve to Save Lives takes lessons from the COVID-19 pandemic and proposes an updated understanding of pandemic preparedness. Moving forward, we must secure increased and sustained funding from governments, while enhancing technical capacities and operational excellence in public health systems worldwide. Strengthening our global health architecture demands a commitment from countries, effective governance, and responsible use of resources. We need strong, accountable global leadership and robust technical support, backed by substantial new funding and efficient financial mechanisms. Ultimately, success hinges on fostering collaboration, recognizing our interdependence, and establishing mutual accountability in our efforts.
A new model for integrating public health and health care delivery— epidemic-ready primary health care—that can identify and stop outbreaks, maintain essential services during disruptions, strengthen population resilience, and ensure health worker and patient safety. For the Lancet Global Health, we argue that strengthening primary health-care capacities for detection, vaccination, treatment, and coordination with public health would improve health security significantly. We anticipate that progress will be stepwise, driven by agreements on core services, optimized funding mechanisms, and health improvement incentives. Advocacy from health workers and civil society will be essential, as is political consensus. To achieve robust epidemic-ready primary health care, we must commit to substantial financial and structural reforms, ensuring that we are prepared for future health challenges.
Large-scale epidemics and pandemics threaten global health security and community resilience, especially concerning emerging infectious diseases and the resurgence of previously controlled conditions. Communities play a vital role in preventing, detecting, and responding to these threats, as demonstrated in recent outbreaks. Effective community involvement enhances government efforts and mitigates negative impacts. This study emphasizes the importance of collaborative partnerships among civil society, the private sector, and government, highlighting that pre-established systems and trust are crucial. Through case studies from the Red Cross and Red Crescent movement, best practices for community engagement in epidemic preparedness and response are presented, showcasing effective participation and joint planning.
In The International Journal of Health Planning and Management, Resolve to Save Lives argues that the amendments to World Health Organization’s International Health Regulations (WHO IHR)—especially the emphasis on multisectoral coordination and strengthening subnational capacities— offer an important opportunity for countries to bolster their public health systems. As demonstrated by the COVID-19 pandemic, it is critical for national legal frameworks to include a coordinating authority and ensure strong capacities at local levels. Adopted at the national level, these legal reforms can make it easier for countries to prevent, detect and respond to health emergencies, improving health security worldwide.
Can the 7-1-7 target increase the number of household contacts (HHCs) of tuberculosis patients initiated on preventive therapy? In this letter published in he International Journal of Tuberculosis and Lung Disease, our colleagues at International Union Against Tuberculosis and Lung Disease describe how the 7-1-7 metric was adapted for TB preventive therapy (TPT), requiring HHCs to be listed within 7 days, screened within 1 day, and started on TPT within 7 days of screening. In a study involving 1,635 HHCs across sites in India, Pakistan and Kenya, the median initiation time for TPT was 6 days. However, persistent challenges included low attendance at health facilities and hesitance among health workers to prescribe TPT, underscoring the urgent need for enhanced support systems and targeted interventions to boost TPT uptake.
While an infection prevention and control initiative improved COVID-19 infection rates for health care workers in Africa, ongoing challenges demonstrated the need for long-term investments in sustainable IPC programs. In BMJ Global Health, Resolve to Save Lives examines an infection prevention and control (IPC) initiative implemented in 22 African countries from April 2020 to January 2021. The initiative provided training, personal protective equipment (PPE) and ongoing supervision to over 42,000 frontline health care workers at 8,444 facilities. Despite achieving short-term improvements in IPC practices, suspected health care worker infections peaked at 41.5% during the pandemic’s first wave in July 2020. The study emphasizes that protecting health care workers requires comprehensive IPC programs, integrated training approaches, enhanced data systems, and sustained investment in PPE.
Nigeria’s experience with a self-assessment of pandemic preparedness underscored the need for investment and stakeholder involvement to strengthen health systems. Writing for Health Security, our colleagues at Nigeria Centres for Disease Control and Prevention reviewed Nigeria’s experience conducting a midterm self-assessment of its pandemic preparedness using a modified World Health Organization (WHO) Joint External Evaluation (JEE) framework and the WHO benchmarks tool. The assessment identified improvements in 11 out of 19 technical areas between 2017 and 2019 and culminated in the development of a 12-month operational plan aimed at enhancing Nigeria’s pandemic readiness.
Effective outbreak response requires sustained investments in health systems—going beyond training to include adequate equipment, space and staffing levels. For Human Resources for Health, our colleagues at ICAP at Columbia University analyzed a COVID-19 response training program for health care workers in 11 African countries in mid-2020. While confidence in managing COVID-19 increased, barriers like limited access to testing kits, PPE, space for isolation, and understaffing persisted.
Trust in authorities, a sense of control over one’s environment and behavior, and access to resources influenced adherence to public health and social measures during the COVID-19 pandemic. Writing in BMJ Open, experts at Resolve to Save Lives analyzed psychosocial and sociodemographic factors influencing COVID-19 public health and social measure (PHSM) adherence through a cross-sectional survey in 18 African Union countries. We found that women, older adults, and those with higher education showed better adherence to personal measures like mask wearing, while rural residents and those with access to running water adhered more to community measures like gathering restrictions. Trust in hospitals, the president, and knowledge about face masks were reliable predictors of adherence. Our findings underscore the importance of building institutional trust and addressing resource disparities to improve adherence in future public health crises.
There is an urgent need for global cooperation, leadership, and sustainable financing to address critical gaps in health preparedness as revealed by the World Health Organization (WHO)’s Joint External Evaluation (JEE). Writing in BMJ Global Health, experts at Resolve to Save Lives highlight the results of WHO’s JEE process, in which 100 countries assessed their ability to handle epidemics and ultimately identified over 7,000 priority actions to address critical gaps. Despite these diagnoses, few actions have been addressed, exposing significant vulnerabilities in global health systems. We emphasize the urgency of strengthening core capacities such as laboratory surveillance and workforce training, as well as the need for global coordination, donor support, and effective leadership to ensure readiness for future outbreaks, as well as more sustainable, long-term financing to bolster public health infrastructure.
There is an urgent need for sustained funding and coordinated global efforts to strengthen health security capacities and prevent future pandemics. Writing in the Journal of the American Medical Association, experts from Resolve to Save Lives analyze critical lessons from the COVID-19 pandemic, highlighting gaps in preparedness that led to millions of deaths, economic losses, and educational setbacks. We stress the importance of building core capacities—prevention, detection, and response—at local, national, and global levels, with particular attention to low-resource settings. We advocate for sustained investment over the next 5-10 years to address these health security gaps, emphasizing that effective global collaboration is the key to preventing future pandemics.
Nigeria’s adoption of the World Health Organization’s Joint External Evaluation (JEE) and National Action Plan for Health Security (NAPHS) will strengthen its national health security efforts. Writing in Health Security, experts at Resolve to Save Lives document the process of completing a JEE with partners in Nigeria in 2017 and subsequently creating a NAPHS to improve prevention, detection, and response in 2018. The process included developing a 5-year implementation plan, creating management teams, drafting outbreak legislation and training professionals at subnational and local levels. Strategic use of international assistance, coupled with reviews of major outbreaks, will strengthen Nigeria’s ability to prevent and respond to health security threats, and regular review and adaptation of its 5-year plan will be essential to ensure sustained progress.
Pandemics are more than public health emergencies; they are multisectoral crises that touch every aspect of public and private life. Therefore, multisectoral coordination—especially by enabling stakeholders to share and coordinate information, resources and personnel—enables appropriate policy responses during crises. Writing in BMJ Global Health, experts at Resolve to Save Lives and our partners identify six low-income and middle-income countries that acted quickly to foster coordinated multisectoral collaboration in their COVID-19 response, which boosted preparedness and action and ensured that policy responses were equal to the magnitude of the crisis. Countries who have demonstrated extraordinary progress provide crucial lessons that should not be ignored as we build a global health architecture that facilitates multisectoral, interdisciplinary, sustainable coordination and cooperation.
SARS-CoV-2 infections among health care workers caused up to 8.38% of total health expenditures in five low- and middle-income countries, underscoring a need for stronger protection measures for frontline workers, who faced increased risk of infection during the COVID-19 pandemic. Writing in Nature Communications, experts at Resolve to Save Lives used a a cost-of-illness (COI) approach to model the economic burden associated with SARS-CoV-2 infections in five low- and middle-income sites (Kenya, Eswatini, Colombia, KwaZulu-Natal province, and Western Cape province of South Africa) during the first year of the pandemic. Our analysis revealed higher infection rates among health care workers compared to the wider population, with significant secondary transmissions and related deaths and impacts on maternal and child mortality. These societal burdens highlight the importance of adequate infection prevention and control (IPC) measures to keep health care workers, and the rest of us, safe during crises.
A targeted investment of $124 billion over five years will enable 196 countries to strengthen their core capacities across the World Health Organization (WHO)’s Joint External Evaluation (JEE) indicators. Writing in PLOS Global Public Health, experts at Resolve to Save Lives estimated the costs required to strengthen country-level health security and identified associated cost drivers. The cost of building public health capacity was estimated based on investments needed, per country, to progress towards “demonstrated capacity” across all WHO JEE indicators. Personnel costs, including skilled health, public health, and animal health workers, are the single most influential cost driver, comprising 66% of total costs. These findings provide cost estimates to inform ongoing health security financing discussions at the global level and highlight the significant need for sustainable financing mechanisms.
The 7-1-7 target supports timely detection, notification, and response to outbreaks. Writing in the Lancet Global Health, experts from Resolve to Save Lives assessed 41 public health events in Brazil, Ethiopia, Liberia, Nigeria, and Uganda between 2018 and 2022 to understand the frequency at which targets for detection (7 days), notification (1 day) and respones (7 days) are being met following implementation of the target. Results showed that 54% met the 7-day detection target, 71% met the 1-day notification target, and 49% completed early response actions within 7 days. Most bottlenecks and enablers were identified at the health facility level, highlighting the need for increased investments in primary health care to enhance outbreak detection and response capabilities.
Revolving outbreak investigation funds (ROIF) can accelerate outbreak response times when coupled with streamlined approval processes. Writing in Health Security, experts from Resolve to Save Lives analyze the impact of ROIF in Nigeria, which were established by our partners at Nigeria’s Centre for Disease Control and Prevention (NCDC) in 2019. Comparing outbreak responses before and after ROIF’s introduction, the median time to response decreased from 6 days to 2 days, highlighting the importance of having immediate access to funds and efficient approval mechanisms during public health emergencies. The study suggests national governments should allocate budgets to sustain such funds, and offers a model for improving outbreak preparedness and response globally.
Strict adherence to infection prevention and control measures, and timely implementation of nonpharmaceutical interventions, can help prevent and control COVID-19. Writing in Emerging Infectious Diseases, experts at Resolve to Save Lives examine the role of superspreading events (SSEs) in the rapid spread of SARS-CoV-2, highlighting their potential to accelerate outbreaks and prolong transmission. We emphasize the importance of timely public health action, particularly in healthcare settings, to identify and manage these high-risk events. Understanding transmission dynamics and implementing strict infection prevention and control (IPC) protocols are critical to preventing future outbreaks.
Frontline health care workers need full protections in the form of infection prevention and control (IPC) measures, water, sanitation and hygiene (WASH) programs, and expanded training opportunities. Writing in the International Journal of Health Planning and Management, experts at Resolve to Save Lives review health care worker infections and deaths during previous epidemics, illustrating the high human and economic costs of neglecting their safety. The study advocates for comprehensive investment to strengthen healthcare infrastructure and cultural shifts to safeguard those on the frontlines of global health crises.
Experts from Resolve to Save Lives expamined the feasibility of adapting the 7-1-7 target to control tuberculosis in Karachi, Pakistan through timely provision of TB preventive therapy (TPT). From January to June 2023, we successfully line-listed 92% of 450 index patients’ household contacts within seven days of initiating anti-TB treatment. Additionally, we determined screening outcomes for 84% of 1,342 contacts within one day. However, we found that only 35% of eligible contacts received further evaluation and treatment within seven days, facing challenges such as travel costs and fear of diagnosis. Our field staff reported that these timeliness metrics motivated prompt action and recommended their integration into national guidelines to improve TB management within households.
In the wake of the COVID-19 pandemic, Resolve to Save Lives collaborated with U.S. jurisdictions to create four digital solutions that enhance the efficiency of case investigation and contact tracing to reduce the spread of infectious diseases by enabling more precise outreach, timely interventions, and better confidentiality: Epi Viaduct, Epi Contacts, Epi Locator, and Epi Viewpoint. Epi Viaduct dramatically sped up the transfer of 7.4 million records from over 2.5 hours to under 1 minute. Epi Contacts improved contact elicitation, resulting in 18,700 contacts from 9,440 index cases. Epi Locator facilitated 134,410 searches with a 75% success rate. These technologies, while developed for COVID-19, can also be adapted for managing any communicable disease.
A modular, self-paced, mobile-friendly online course on foundational infection prevention and control (IPC) was developed for health workers (HWs) in Africa, addressing challenges in accessing training. Evaluated in Nigeria, the course comprised 10 modules utilizing IPC vignettes and short assessment questions. Of the 372 learners who enrolled, 59% completed all modules, demonstrating significant pre-test (29%) to post-test (54%) score improvements (effect size 1.22). User experience was rated positively, with a Net Promoter Score of +62. These results suggest that scalable online training can effectively bridge IPC knowledge gaps among HWs in the region.
Public health emergencies such as COVID-19 and other large-scale outbreaks (cholera, measles, and mpox) are occurring with increasing frequency, magnitude, and complexity, compounded by devastating natural disasters, conflicts, and other humanitarian crises. Timely and effective intelligence is vital for decision-makers to assess risks, prepare, and respond appropriately. Experts from Resolve to Save Lives and partners discuss how collaboration across sectors is essential to strengthen integrated disease surveillance and ensure timely and effective solutions to global challenges.
Our report details the problems affecting our health care workforce and key actions that governments, health systems and funders must take to address them.
Engaging local governments in epidemic preparedness will strengthen global health security by ensuring better coordination between local and national authorities. Writing in PLOS Global Public Health, Resolve to Save Lives and partners explore local-level involvement in epidemic preparedness before the COVID-19 pandemic. The research, based on responses from 33 cities in the Partnership for Healthy Cities, shows that while national governments played a dominant role in preparedness, many cities conducted vital risk assessments and developed response plans. By incorporating local governments more actively in future preparedness efforts, we can better coordinate responses for stronger overall health security.
While long-term planning for health security is indispensable, focused short-term operational planning can be a tremendous asset for developing actionable and realistic strategies to improve readiness for public health emergencies. Despite limited funding and an overwhelming list of action items, Uganda successfully enhanced its epidemic readiness by 20% with a focused 1-year operational plan developed after a rapid self-assessment, tackling 72 of the 264 activities in their 5-year NAPHS. By concentrating on a smaller number of high-impact activities, Uganda demonstrated that it is possible to strengthen long-term health security capacities with focused short-term planning, showcasing a model for other countries facing similar challenges.
The COVID-19 pandemic was the most disruptive global health crisis in a century. Analysis of publicly available data by experts from Resolve to Save Lives revealed that alongside preparedness capacities, governance and leadership capacities independently contributed to lower COVID-19 cases and deaths. Both preparedness and governance are essential for effective pandemic control, requiring stronger public health systems and leadership.
This briefing note explains why alert-level systems for COVID-19 are effective, compares models from several countries, and provides the key principles and potential pitfalls to be aware of when developing these systems. It is intended to provide guidance to local, regional and national governments on best practices for alert-level systems, and on how to clearly communicate what behaviors people should adopt in response to changing COVID-19 conditions in their community.
Identiftying critical points of failure within the health system and during emergencies is the first step to mitigating future risk exposure. The West African Ebola epidemic (2014-2016) revealed alarming gaps in infection prevention and control for health care workers, highlighting a major vulnerability in global health security. Experts from Resolve to Save Lives propose a two-pronged soluion: prioritizing IPC as a global epidemic preparedness measure and conducting rapid risk assessments to adapt strategies for health care worker protection. Improved global support and targeted interventions are vital to strengthen health systems and safeguard frontline workers.
Timeliness is essential in preventing and controlling infectious diseases like meningococcal meningitis and tuberculosis (TB). Experts from resolve to save lives explored adapting the global 7-1-7 target for outbreak control to the management of household contacts of TB patients. Applying the metric in India, Pakistan, and Kenya improved TB preventive therapy (TPT) initiation rates, though logistical and health care barriers persisted. Field staff recommended a “3-5-7” metric to enhance screening and TPT delivery. Timeliness metrics provide structure and urgency, offering a valuable tool for improving HHC management and global TB prevention efforts.
In a roundtable discussion with health practitioners, funders, academics, and policy-makers, experts from Resolve to Save Lives identified key areas for improving global health practices. We emphasized the importance of evidence-based frameworks that are adaptive and responsive to prioritised health needs. Key recommendations include enhancing information-sharing, increasing social engagement, and promoting diversity in decision-making processes. We also highlighted the need for collaboration with both hyperlocal and global entities to strengthen global health capabilities. Since pandemic drivers extend beyond the health sector, integrating expertise from various fields is crucial for effective decision-making. We outline seven points to improve evidence-based prioritisation and enhance global health outcomes.
Implementing the International Health Regulations (IHR 2005) can be a cumbersome process, and costs vary widely from country to country. To support facilitating this complex work, experts from Resolve to Save Lives tested several new tools designed to estimate the resources needed for implementing the IHR. Using Nigeria’s National Action Plan for Health Security (NAPHS) as a case study, we compared cost estimates generated through the World Health Organization (WHO) Costing Tool, Georgetown University’s IHR Costing Tool, and CDC’s Priority Actions Costing Tool (PACT). While the tools suggested similar activities for implementation, cost estimates varied due to differences in procurement and human resource needs. We found that a strategic approach, prioritizing major cost drivers based on resource availability, could help accelerate the implementation of health security plans.
Clear, universal performance standards for outbreak detection, reporting and control can improve accountability, save lives, and accelerate global readiness for future pandemics. For The Lancet’s Viewpoint, experts from Resolve to Save Lives propose 7-1-7 as a global target for timely response to infectious disease outbreaks: detecting a suspected outbreak within 7 days, reporting and initiating a response within 1 day, and mounting an effective early response within 7 days.