
High blood pressure is the world’s deadliest condition—and the most neglected. But last September, as world leaders gathered for the United Nations General Assembly in New York, I joined WHO Director General Dr. Tedros Ghebreyesus and Mike Bloomberg to launch WHO’s first ever global report on hypertension.
Pandemics, as COVID-19 reminded us, can kill tens of millions of people and cost the global economy trillions of dollars. In 2023, the 7-1-7 Alliance was born, a new country-led global partnership to prevent epidemics. WHO adopted the 7-1-7 target as part of its new guidelines on early detection and early response.
Our vision: preventing 100 million deaths from cardiovascular disease and making the world safer from epidemics.
I found these to be inspiring, pivotal moments that will make 2023 a turning point toward a healthier, safer world.
I found these to be inspiring, pivotal moments that will make 2023 a turning point toward a healthier, safer world.
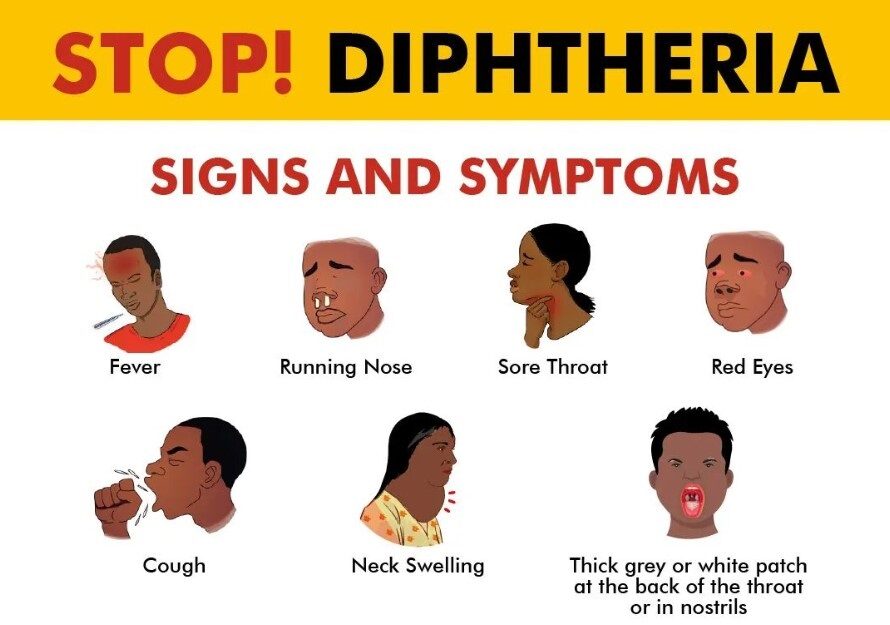
The challenges we face can seem overwhelming: Climate change and other environmental crises, wars, political polarization, poverty and inequality, epidemics of obesity and drug addiction, resurgent infectious diseases, antimicrobial resistance, and more.
Without minimizing the reality of these deadly and potentially worsening trends, I remain optimistic. Doctors, nurses, pharmacists, public health specialists, community health workers and others around the world are protecting and improving peoples’ lives every day. New technologies advance our ability to improve health. And despite polarization and media portrayals, there’s strong consensus on the need for more support for public health. Some of the many positive trends:
- Our call for the elimination of artificial trans fat from the global food supply has driven progress. We’ve supported a nearly six-fold increase in people protected since we and WHO launched the REPLACE technical package in 2018. Today, there are 3.7 billion people in 56 countries that are being protected.
- We worked with our partners in Democratic Republic of Congo and Nigeria to establish Rapid Response Funding mechanisms, distributing small but crucially important funds to subnational levels—where outbreaks begin and can be ended. This led to faster responses and better outbreak containment efforts.
- With nearly 20 million patients treated since RTSL programs began, countries are building scalable, life-saving programs that make it easier for patients to control their high blood pressure. Our innovative approach to making data systems simple and powerful has empowered health care workers to provide better care for patients.
- The cardiovascular health program we support in China facilitated improvement in the label on low-sodium salt, removing a large barrier to the promotion of these life-saving products.
- Nearly 200 public health leaders from throughout Africa have participated in our Program Management for Epidemic Preparedness process. Through peer exchange and experiential learning, teams of leaders are accelerating improved preparedness.
We’re delivering on our promise to partner with countries as they protect and improve healthy lives.
Two hundred years ago, no one imagined that typhoid, plague, tetanus, and other infections would be gone in much of the world and receding in the rest. I’m confident that heart disease and stroke will—in the not too distant future—be as rare as those once common killers are today.
We and, most importantly, the people we serve appreciate and need your continued commitment, involvement, and support.
Thank you.
Dr. Tom Frieden
President and CEO
Resolve to Save Lives

Public health that delivers on its promise
One country at a time, we’re building a healthier future together. If a strategy works—we work with our partners to take it to scale.
That’s how we resolve to save lives.

Expanding global access to treatments, processes and data systems that work.
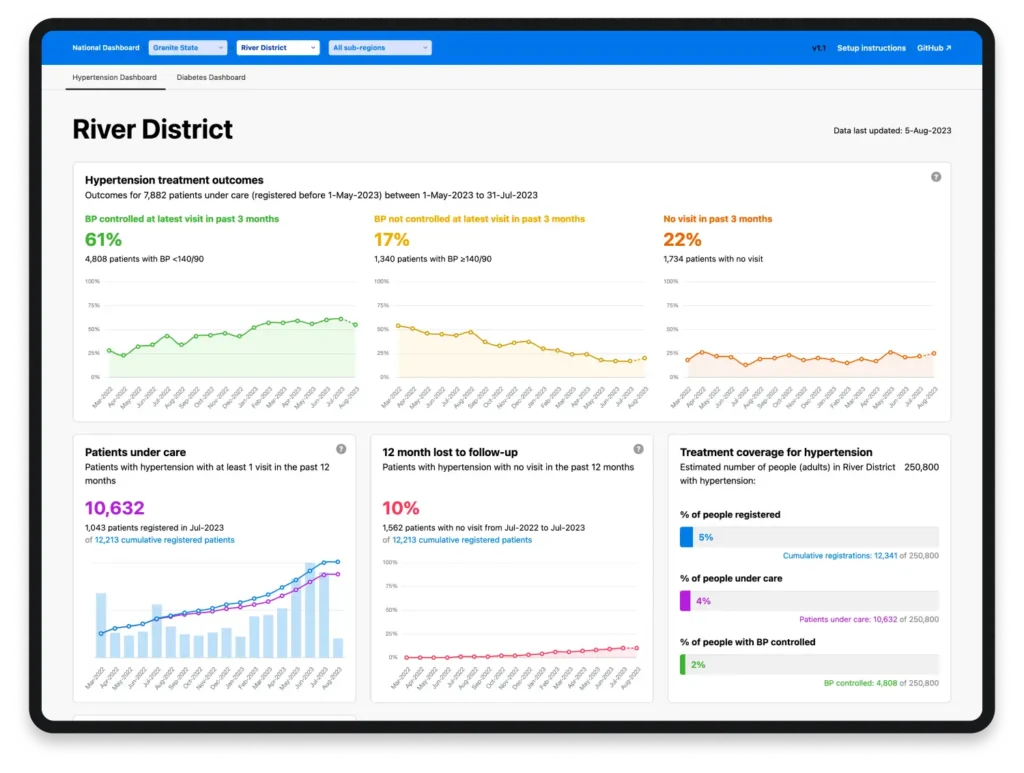
facilities equipped to provide high-quality hypertension care
of patients with blood pressure under control within the last 3 months
Bangladesh nearly tripled its control rate for high blood pressure (from 20% to nearly 60%) and expanded access to life-saving treatment to millions.
We worked with partners to learn how dedicating focus on people and processes can revolutionize epidemic preparedness. We’ve now trained over 200 public health experts to lead lasting progress in global health security.
Supporting health care workers with fit-for-purpose tools, accessible and up-to-date training, and safer working conditions.

We partnered with WHO to make Infection Prevention and Control a national priority in Senegal, Cote D’Ivoire, Guinea, South Sudan. Madagascar and Rwanda.
We worked with the World Bank to demonstrate just how much it costs economies when we fail to protect our health care workers.
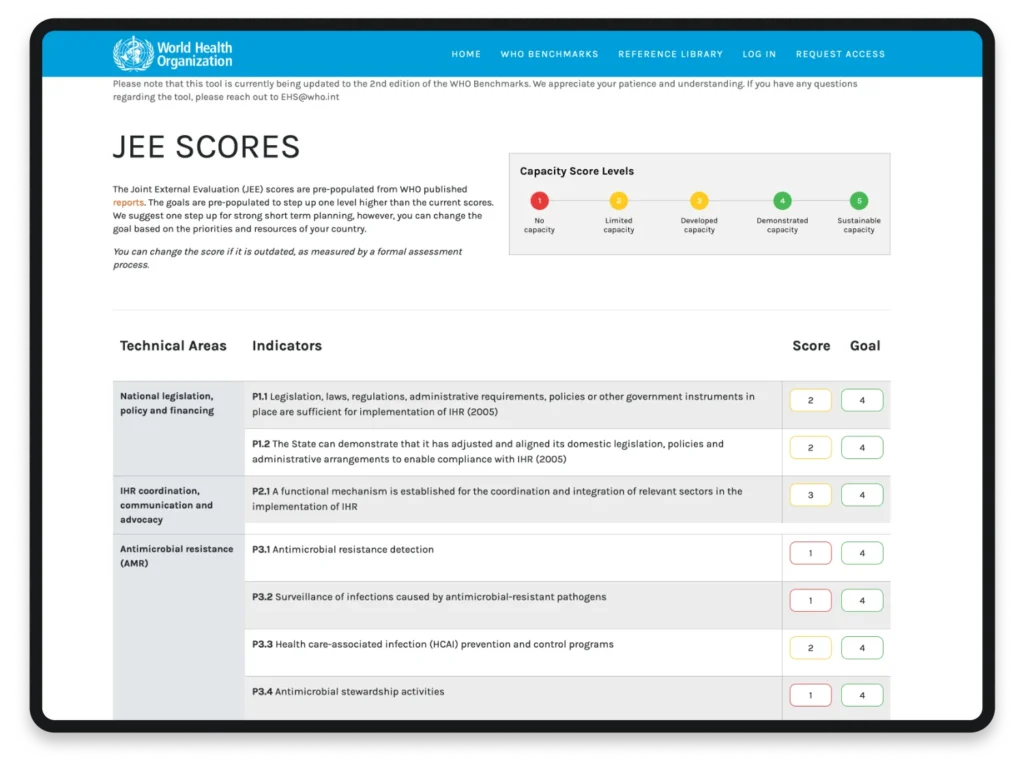
We collaborated with WHO-HQ on a digital tool that can shorten the time it takes to plan for International Health Regulations (2005) from months to minutes.
Building better, more resilient health systems prepared for whatever the future holds.

The countries we partner with have demonstrated substantial improvements in their ability to detect and respond to public health risks, as independently evaluated by WHO.
We launched our Epidemic-Ready Primary Health care program, because primary care is our first line of defence in public health.
International organizations can sometimes forget that global health security begins at the country level. We’re working hand-in-hand with country governments to strengthen the architecture of public health systems.

The heart of the matter
We’re leading the charge to get high blood pressure under control.
with a system that works for 32 countries and over 19 million patients…and counting.
HEARTS celebrated 5 years of saving lives this year 🎂
On the global stage: WHO released its first-ever global report on hypertension.

We documented how including high blood pressure treatment at HIV clinics can improve hypertension care and prevent heart attacks and strokes.
Our call for the elimination of artificial trans fat from the global food supply has driven progress.
In 2023, Pakistan, Nigeria, Egypt, Sri Lanka and Mexico all passed trans fat elimination policies to protect a combined 702 million people.
With our support, nearly 6x more people globally have been protected from trans fat exposure since we helped launch REPLACE in 2018.

To celebrate countries for their efforts and encourage long-term enforcement, we collaborated with WHO to launch a Trans Fat Elimination Validation Programme.
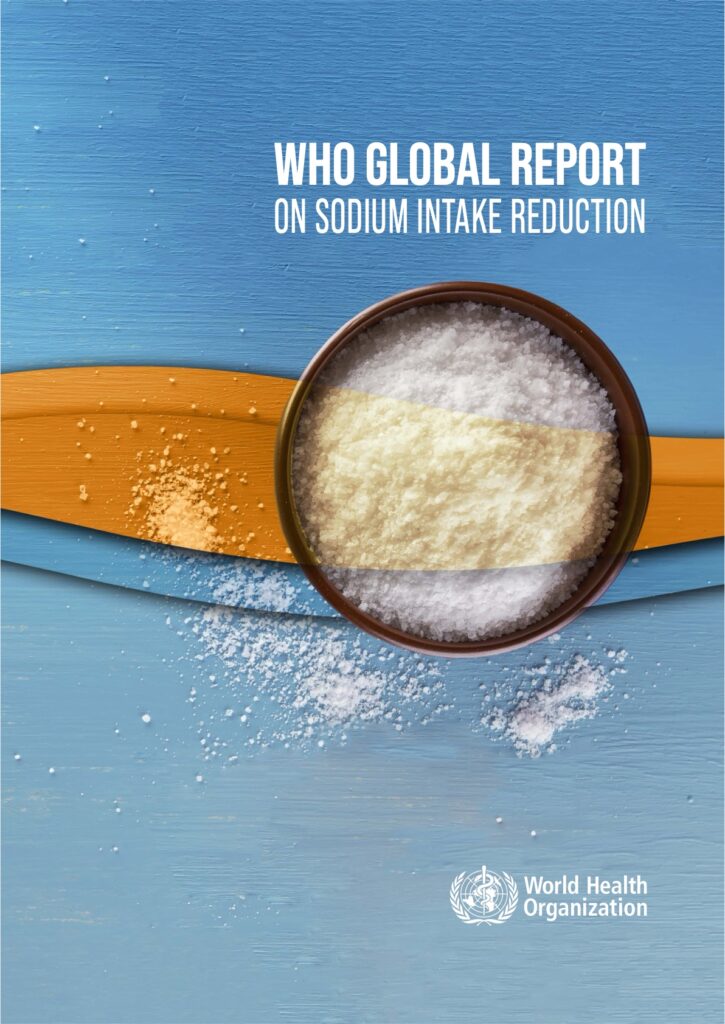
We have innovative ideas for reducing the world’s dangerously high salt intake.
We worked with WHO on a landmark report that found we can save 7 million lives by 2030 with smarter policies.
Replacing regular salt with low-sodium salt is a revolutionary strategy for lowering sodium and saving lives. Singapore pioneered this approach in 2023, and we spread the word.
Heart health starts with healthy nutrition. This year, Nepal passed nutrition standards for public schools, and India scaled a successful pilot cutting salt in school lunches to protect the health of more than 5 million children.
Better and faster at preventing epidemics
We support global network of epidemic-ready countries that don’t just respond to outbreaks—they get ahead of them.

Redefining “early warning”

“Early warning” used to mean we’d caught a virus that was already starting to spread. We’ve partnered with Nigeria, Uganda and Ethiopia to demonstrate how countries can monitor risk. plan ahead and nip outbreaks in the bud.
We’re applying design-thinking to public health— partnering with countries to develop innovative solutions. In Zambia, a week-long design sprint resulted in a prototype for a new digital event management system.

7-1-7 became synonymous with speed—and continuous improvement.
In February, we launched The 7-1-7 Alliance: a new country-led, global partnership committed to preventing epidemics.

WHO made the 7-1-7 target the bedrock of its new guidelines on early detection and early response.
WHO made the 7-1-7 target the bedrock of its new guidelines on early detection and early response.
The 7-1-7 Alliance founded a community of practice with 15 countries and counting to share learnings and spur innovation to accelerate global progress
Next-generation epidemic preparedness

We’ve started working in four countries to make primary health care facilities “epidemic-ready” —ensuring they can respond effectively to outbreaks while maintaining essential services.
Our partners are learning how to overcome administrative barriers to unlock millions in pandemic preparedness and response funds—and put them to good use.
This year, at the request of several countries, we offered legal guidance to support them in their efforts to improve infectious disease control.
Better data for life and death decisions
Going digital
Making paper records a thing of the past
High loss to follow-up is a common problem with hypertension care, which requires regular visits. Going digital allowed Bangladesh to automate reminders and triple the percentage of patients who stuck with the program.
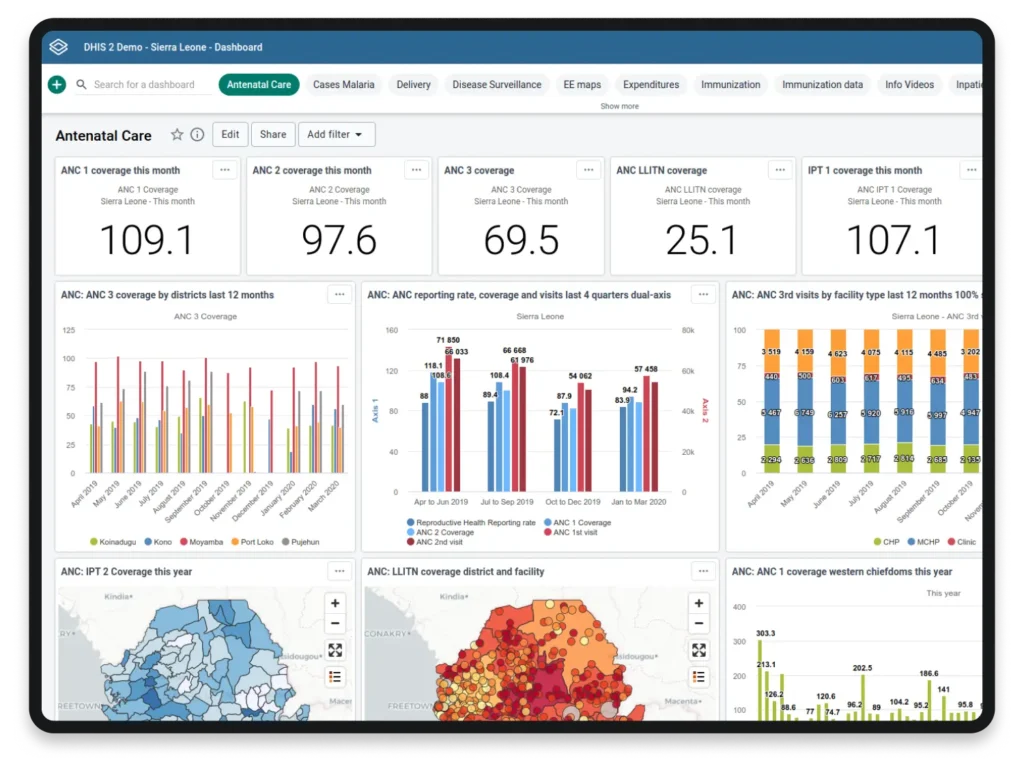
DHIS2 is the biggest health information system in the world. We worked with the University of Oslo to make the DHIS2 Tracker app faster and easier for health care workers to use.
We helped mobilize over 100 partners from public and private sectors and academia to invest in and provide thought leadership, technical guidance and support for Africa CDC’s Digital Transformation Strategy.
Going global
We spotlight local successes, amplify innovations and support collaboration between countries so that public health lessons can be shared worldwide.

The 70+ participants in this year’s PMEP program went home to their 12 respective countries equipped with the knowledge and networks to accelerate preparedness efforts and protect over 500 million people from future epidemics.
We created a free database providing centralized access to nutrient data in packaged foods from around the world to create transparency around high levels of sugar, salt and saturated fat in popular food products.


Countries still considering adopting trans fat elimination policies wanted to know what implementation and enforcement would really look like. We released a series of case studies from around the world to show them: it can be done.
Tools that work for health care workers
And provide actionable data for health programs
Simple’s HEARTS360 dashboard enables countries to better visualize, monitor and interpret data from their chronic disease management programs—and make them more effective at saving lives.
The Simple app got an upgrade: new features improve program management for chronic disease care and send alerts for medication stockouts.
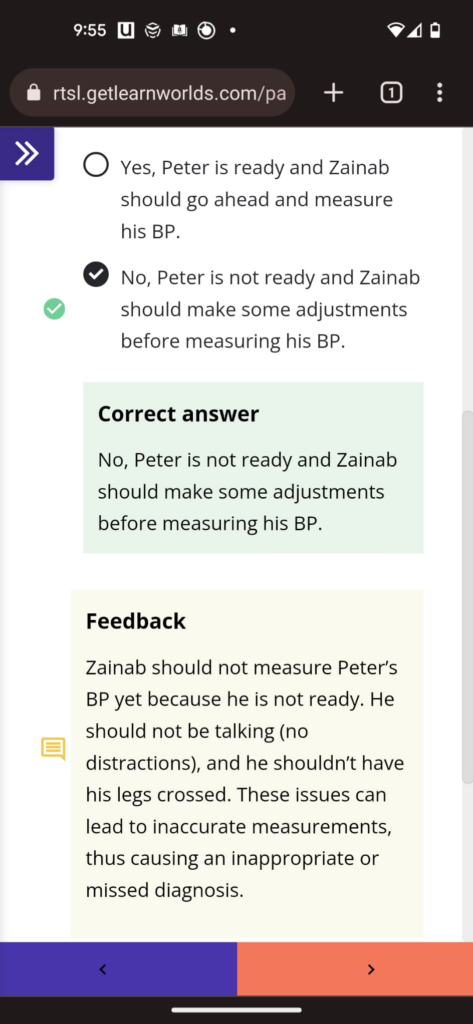
We’re pioneering mobile-first, self-paced online training programs keeping health care workers up to speed, on the go.
Making progress possible

We answer the call
No matter where we’re asked to go, we recruit the right people and build programs that make an impact.
Our team of 150 employees spans across 10 countries and partnership agreements with 59 countries. And we’re just getting started.
RTSL Nigeria was inaugurated in 2022, and in 2023 we registered in Ethiopia, welcoming a team of 19 staff leading life-saving programs and sharing best practices with the global community.
Our RTSL Ethiopia team, with the support of essential partners, is implementing life-saving programs and sharing best practices with the global community—improving health for the people of Ethiopia and the world.
— Dr. Tom Frieden
Audited financials: 2022
Resolve to Save Lives became operating as an independent organization in March of 2022—this section covers our first nine months of operations, March-December 2022.
None of this progress would be possible without the support of our donors:
Skoll Foundation
Tambourine
Founder’s Pledge
Lyda Hill Philanthropies
Wellcome Trust
Atria Health Collaborative
$44M
Our total operating budget for 2022.
We invested:
Preliminary financials: 2023
With the funding entrusted to us, we strategically allocate our resources to maximize impact for our partners and drive progress in global public health.
Financial information presented for 2023 represents preliminary analysis; final data and audited financial information for 2023 will be posted when available.
Starting in 2024, we’ll be covering just our past year’s financials in our annual reports.
$55M
Our total operating budget for 2023.
We invested:










Thank you to our visionary Boards of Directors for your leadership and support.
We still need your help
We’re known for making the most of the funds entrusted to us. Dr. Salam Gueye, Director of Emergencies for the World Health Organization Africa Region said:
$50,000 from Resolve to Save Lives is often more valuable than millions from another donor.

Since 2017 we have made tremendous progress with our partners. But to save 100 million lives over the coming decades, we need your help today.