Resource Library
Primary health care
Resolve to Save Lives
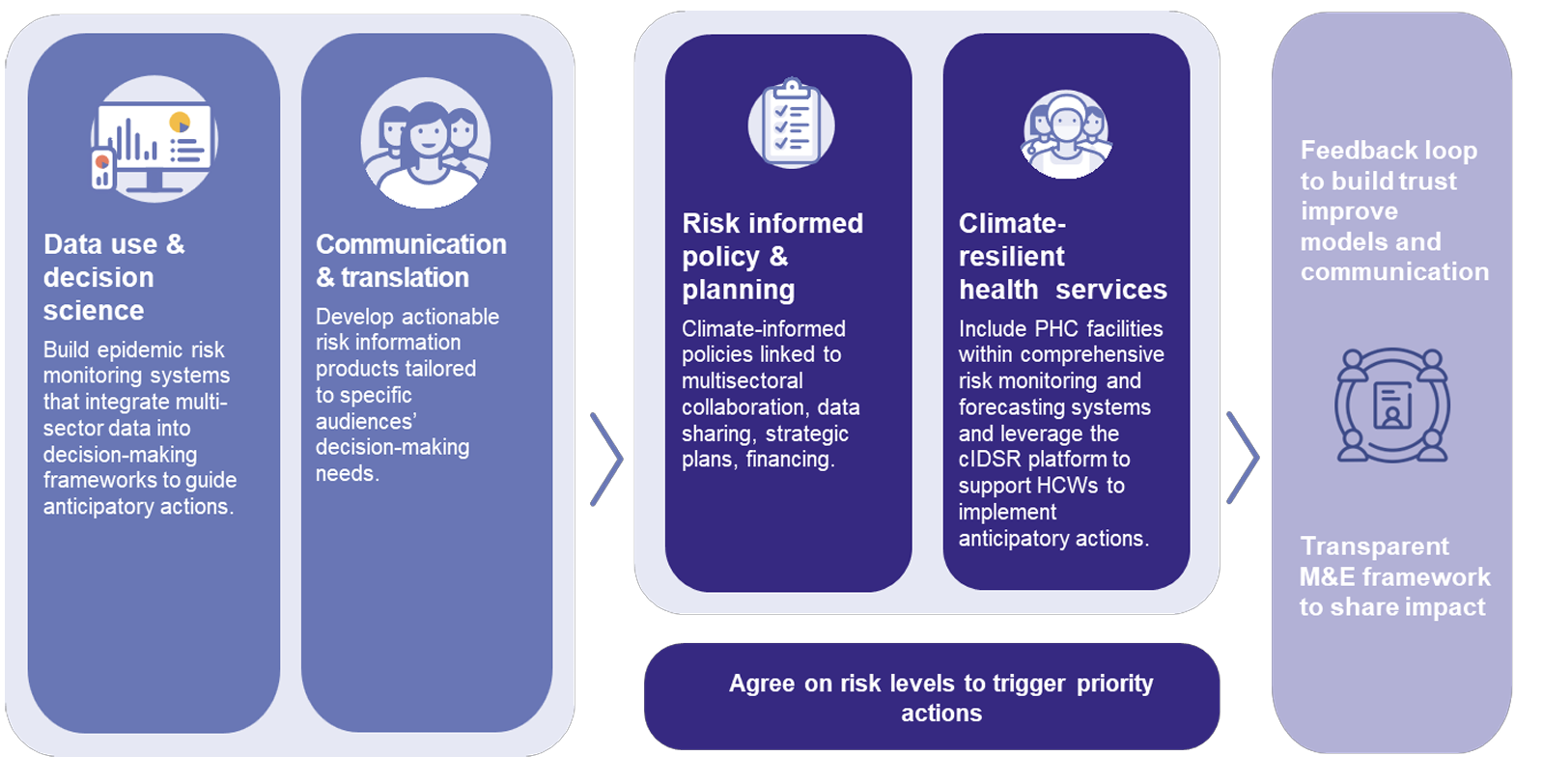
Strengthening epidemic readiness by integrating climate data into health systems.
Resolve to Save Lives and Jacobs Solutions
Our blueprint for strengthening primary health care infrastructure to withstand epidemic and climate threats.
Resolve to Save Lives
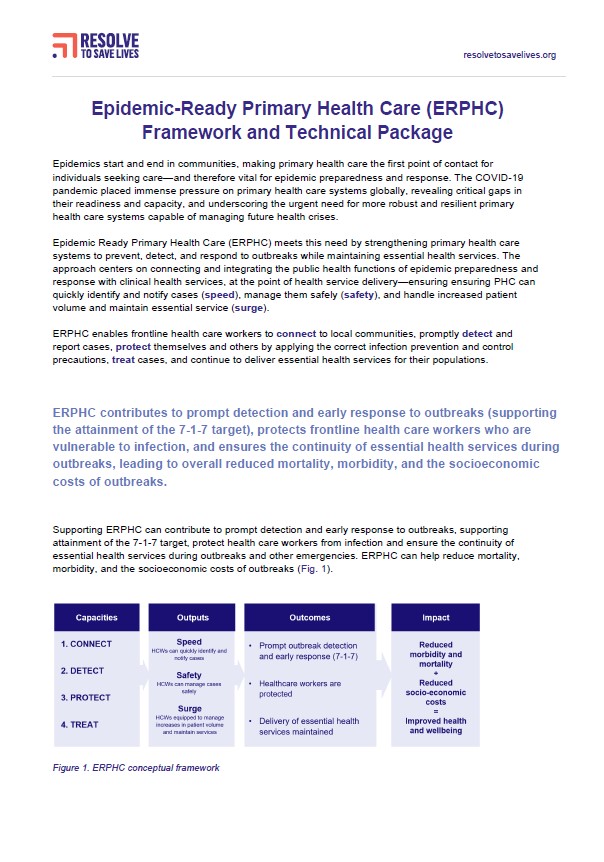
Capacities, core activities and outcomes for implementing Epidemic-Ready Primary Health Care (ERPHC).
Resolve to Save Lives
Resolve to Save Lives
The Lancet Public Health
We propose an epidemic-ready primary health care model to integrate public health and health care, stop outbreaks, ensure essential services, strengthen resilience, and protect workers and patients.
BMJ Global Health
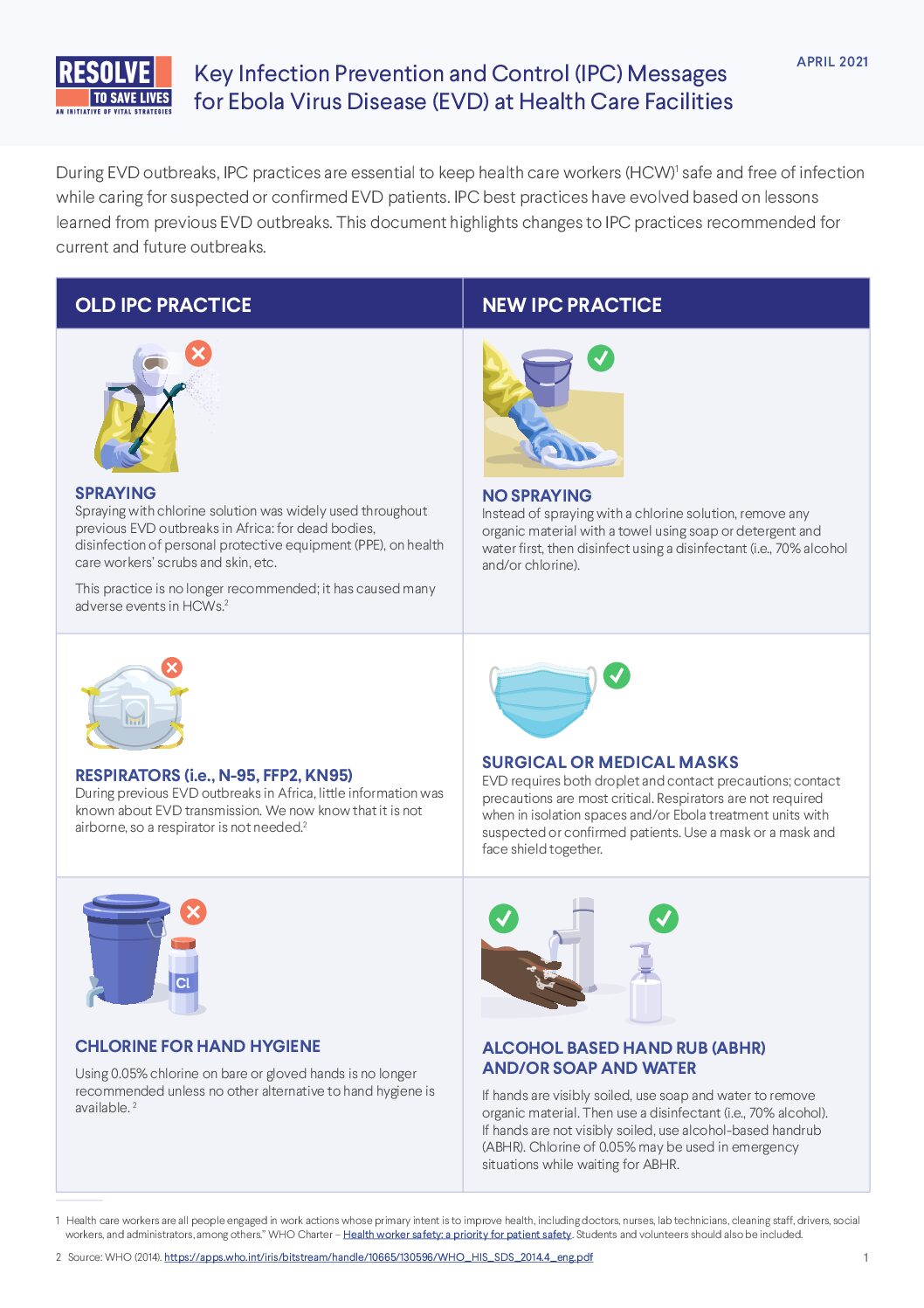
An infection prevention and control initiative improved COVID-19 infection rates for health care workers in Africa, but challenges showed the need for long-term investments in sustainable IPC programs
Human Resources for Health
Effective outbreak response requires sustained investments in health systems—going beyond training to include adequate equipment, space and staffing levels.
Nature Communications
SARS-CoV-2 infections among health care workers caused up to 8.38% of health expenditures in five low- and middle-income countries, underscoring a need for stronger protection measures.
The International Journal of Health Planning and Management
We make the case for expanding health care worker protections, including infection prevention and control measures, water, sanitation and hygiene programs, and expanded training opportunities.
BMC Public Health
How can we keep health care workers up-to-speed and prepared to respond to emerging health threats? For BMC Public Health, we demonstrate the power of self-paced, mobile-friendly training.
Health Security
The 2014-2016 West African Ebola Epidemic exposed a critical weakness in global health security: inadequate protections for health care workers put all our lives at risk. Here’s what we do to fix it.