Resource Library
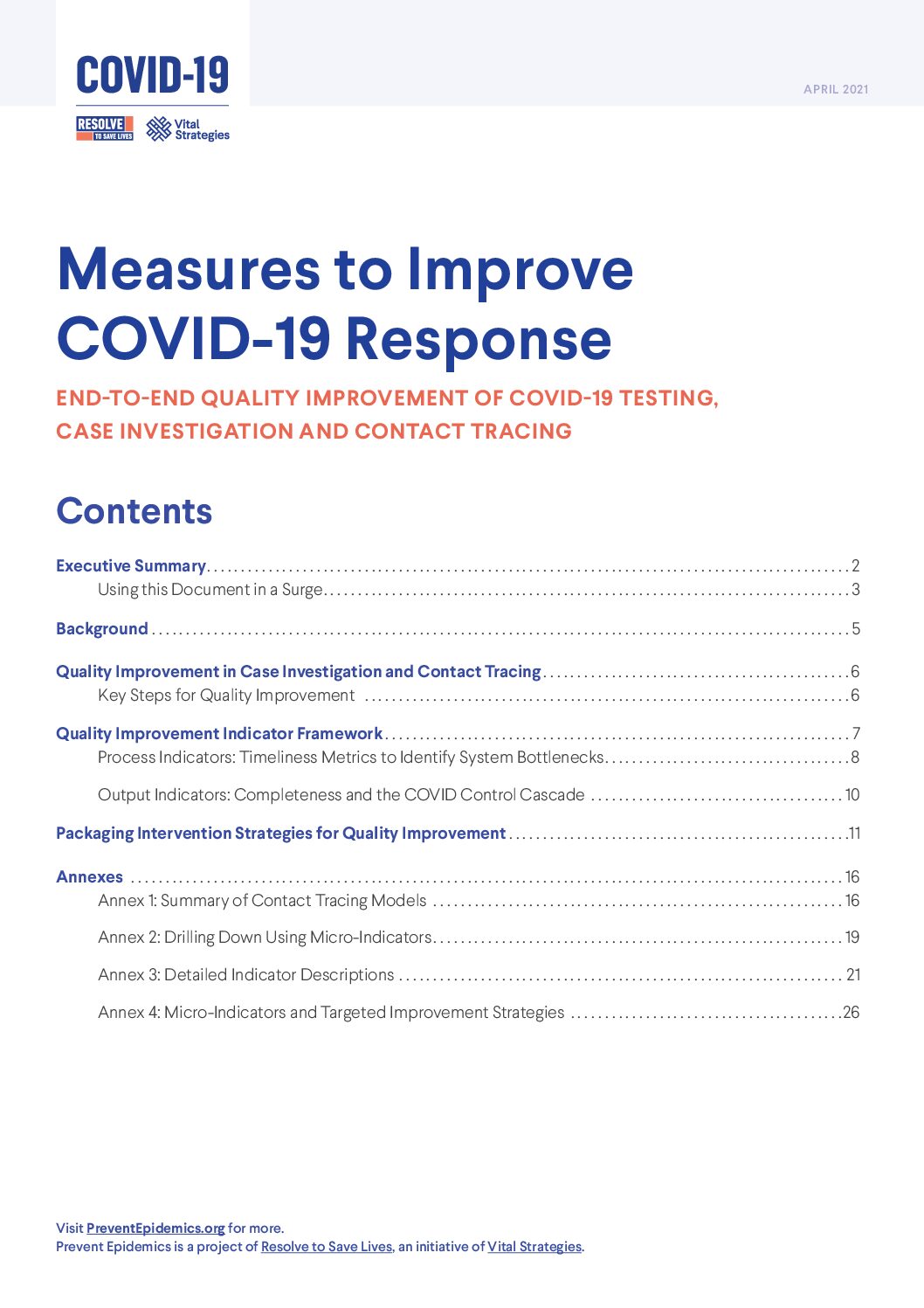
COVID-19
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
Resolve to Save Lives
PLOS Global Public Health
How do local governments contribute to pandemic response? Surveying 25 cities, we documented a crucial role in risk communication and community coordination.
BMJ Global Health
Preparing for the next pandemic requires sustained government funding, efficient financial mechanisms, better public health capacity, strong global leadership, and a commitment to collaboration.
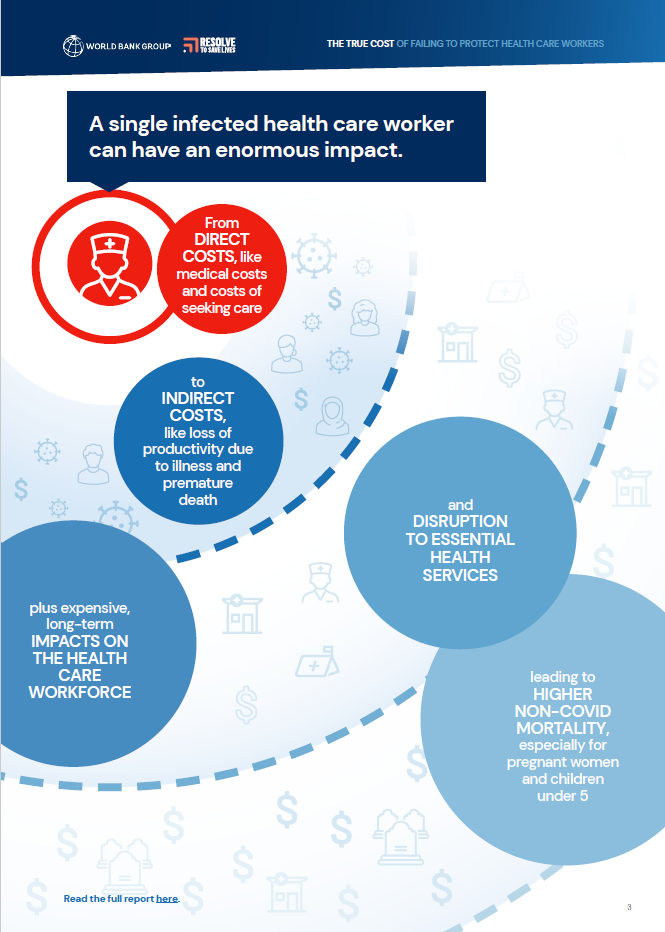
The World Bank, Resolve to Save Lives
A landmark study from the World Bank and Resolve to Save Lives that measures the broader socio-economic costs of health care
worker infections and deaths from COVID-19
BMJ Global Health
An infection prevention and control initiative improved COVID-19 infection rates for health care workers in Africa, but challenges showed the need for long-term investments in sustainable IPC programs
Human Resources for Health
Effective outbreak response requires sustained investments in health systems—going beyond training to include adequate equipment, space and staffing levels.
BMJ Open
Trust in authorities, a sense of control over one’s environment and behavior, and access to resources influenced adherence to public health and social measures during the COVID-19 pandemic.
Journal of the American Medical Association
We emphasize the urgent need for sustained funding and coordinated global efforts to strengthen health security capacities and prevent future pandemics.
BMJ Global Health
We make the case that multisectoral coordination, especially by enabling stakeholders to share and coordinate information, resources and personnel, enables appropriate policy responses during crises.
Nature Communications
SARS-CoV-2 infections among health care workers caused up to 8.38% of health expenditures in five low- and middle-income countries, underscoring a need for stronger protection measures.
PLOS Global Public Health
We make the case for a targeted $124 billion investment over 5 years to enable 196 countries to strengthen core capacities across the World Health Organization’s Joint External Evaluation indicators.
Emerging Infectious Diseases
We argue that strict adherence to infection prevention and control measures, and timely implementation of nonpharmaceutical interventions, can help prevent and control COVID-19.