You’ve been redirected from preventepidemics.org.
Prevent Epidemics is part of resolvetosavelives.org.
How we save lives / Epidemic prevention / Health Care Workers & Epidemic Preparedness
Health care workers & epidemic preparedness
Health care workers are on the frontlines of epidemics and carry the greatest burden.

PPE Training in Ethiopia
Yet even as we celebrate them as heroes, we fail to keep them safe. They face a disproportionately high risk of illness and death, as well as isolation and even stigma. The cascade of burdens health care workers face during a public health crisis played out yet again during COVID-19: insufficient personal protective equipment, fatigue, hundreds of thousands of infections, harassment and stigmatization by the public as well as an uptick in mental health issues and suicides.
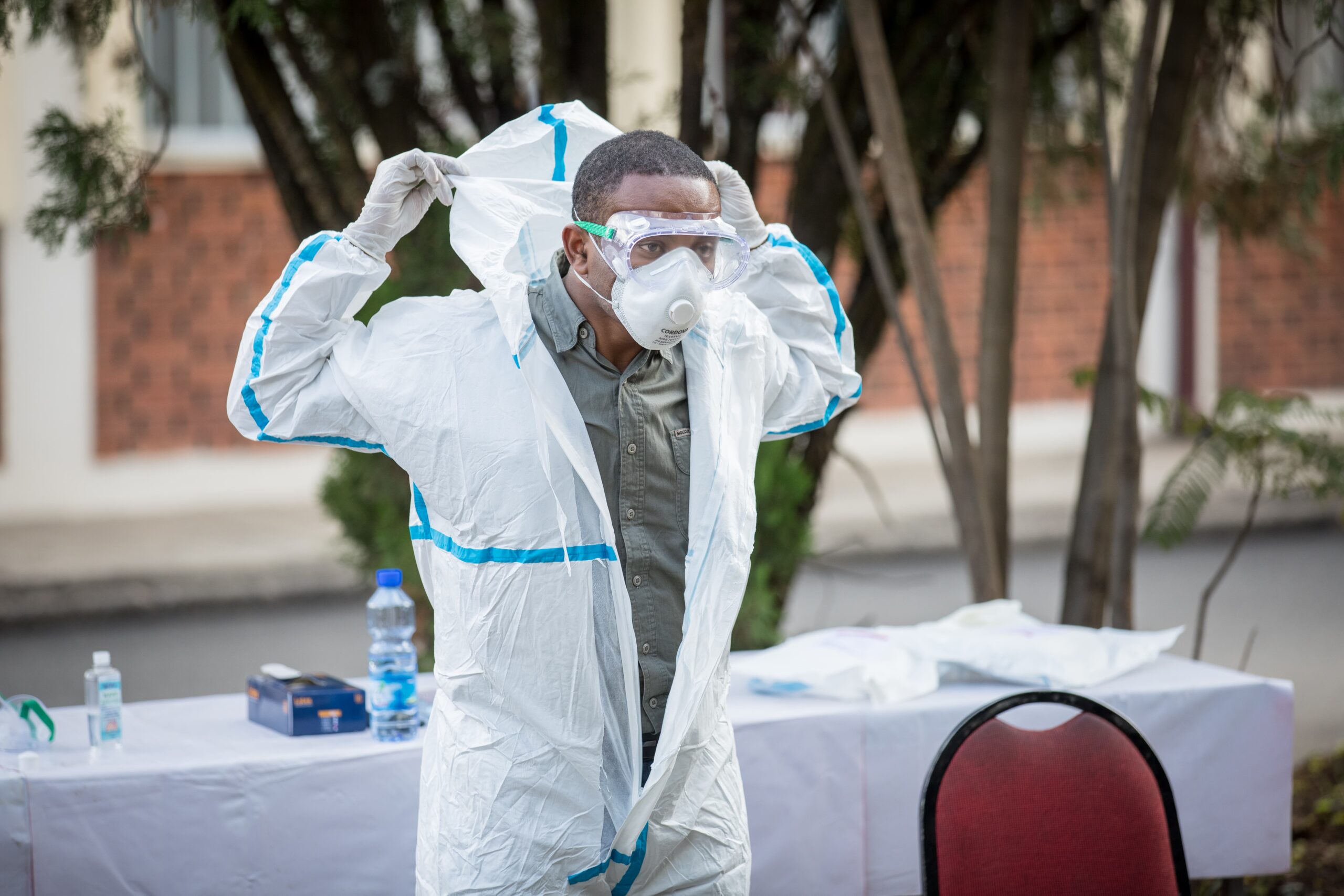
A health care worker in Ethiopia demonstrates how to use COVID-19 personal protective equipment as part of the emergency response initiative Resolve to Save Lives developed and implemented with ministries of health and civil society organizations in 22 African countries
Up to 180,000 health care workers have died during the COVID-19 pandemic*.
*as of September 2021, WHO estimated range of 80,000-180,000
This is not unique to COVID-19. The lack of preparedness for outbreaks of all sizes and refusal to adequately protect health care workers creates a domino effect causing disruptions to — if not outright collapses of — health care systems.
Protecting health care workers requires a range of interventions. Governments and donors across the world must prioritize:
Full implementation of Infection Prevention and Control (IPC) and Water, Sanitation and Hygiene Standards (WASH)
Investing in training, tools and resources for a safer health care workforce
Using and improving tools to monitor implementation of WHO monitoring frameworks at the national and facility levels and enact further improvements in meeting IPC standards
Improving data collection and accountability regarding health care worker infections and deaths
Increasing donor support for and focus on health care worker protections

Learn more about these interventions in our report, Protecting Health Care Workers: A Need for Urgent Action
Protecting health care works during COVID-19
When COVID-19 struck, we partnered with ministries of health and civil society organizations in 22 African countries to develop and implement an emergency response initiative to improve health care worker safety through a comprehensive program including in-service training, data collection and procurement of personal protective equipment (PPE).
Between April 2020 and January 2021, the initiative trained more than 40,000 health care workers from more than 8,000 facilities in 22 countries. As the pandemic progressed, RTSL and country partners continued work to improve infection prevention and control measures and ensure the maintenance of essential health services at the primary health care level at more than 1,800 facilities in nine countries.
…the initiative trained more than 40,000 health care workers from more than 8,000 facilities in 22 countries
A key tenet of the initiative was supportive supervision — a mentorship-based approach to management that prioritizes respect, transparency and collaboration between supervisors and supervisees and involves extensive and open communication.
Participating facilities’ average infection prevention and control scores increased from 66% to 90% as measured by our COVID-19 checklist for primary care facilities. The program also saw improvements in PPE availability and health care workers’ behaviors.
As the world emerges into a new normal following the pandemic, we are continuing to build on the program by working with global partners to build momentum to ensure that the safety of health care workers remains a priority issue in epidemic preparedness.
Learn more about the emergency response initiative’s success, as well as how we’ve transitioned it into our core preparedness work, through stories from some of our implementing partners:

Supporting health care workers to promote service continuity during the COVID-19 pandemic in Ghana

Empowering Medical Staff to Prevent and Control COVID-19 in Sierra Leone

Training the Trainers: Securing the Foundation of an Effective COVID-19 Response in Liberia

Democratic Republic of Congo: Addressing Complex Health Challenges through Preparation and Training
HEALTH HEROES
The Faces of Infection Prevention and Control
We spoke with health care workers from Liberia and Ghana about the real human impact strengthening infection prevention and control has.
Learn about their challenges and successes in promoting infection prevention and control measures during the pandemic.

Preparing for the next pandemic by protecting health care workers
The world can’t afford to lose its health care workforce because of unsafe working conditions. Health care workers require extensive training and can’t be easily replaced. And we’re already facing a global shortage of health care workers — the World Health Organization estimates that an additional 18 million will be needed in the next decade.
Modest investments in health facilities and health care workers will contribute to stronger global health security and make the world safer from the next epidemic threat. For example, a recent WHO report found that improving hand hygiene in health care settings saves about $16 in expenditures for every $1 invested. That same report found that avoidable infections in health care settings were reduced by up to 70% following implementation of IPC practices. This reduction came regardless of whether a country was a high-, middle- or low-income country.
Improving hand hygiene in health care settings saves about $16 in expenditures for every $1 invested.
But there is still substantial work to be done. One in three health care facilities lack proper hand hygiene supplies at the point of care. A 2019 WHO survey could not identify any health facilities in low-income countries with the minimum IPC requirements in place, and found that even in high-income countries, less than 20% of tertiary health facilities met the standard. A recent survey of 106 countries found that only four met the minimum requirements for IPC.
We must invest in health care worker safety now – our ability to prevent the next pandemic depends on it.
Read about how a community health worker worked with a community in rural Kenya to stop an anthrax outbreak in its tracks
Narok, Kenya. Courtesy: International Federation of Red Cross and Red Crescent Societies / The Kenya Red Cross Society
Tools, trainings & resources for health care workers
We invited health care workers who completed our self-advocacy course to tell us about an issue that matters to them. Hear their voices.
Self-Advocacy for Health Workers
The course covers essential self-advocacy and storytelling skills that you can use to make the case for change on an issue that matters to you, with a focus on issues affecting HCW safety. Issues might include access to vaccines and running water, or ensuring that health facilities have enough personal protective equipment (PPE) to protect all HCWs. The course features short videos created by the Community Health Impact Coalition and the Stanford Center for Health Education.
IPC Foundations
This self-paced course focuses on foundational concepts in infection prevention and control (IPC), with a focus on practices applicable to primary health care facilities in Africa. This training covers common questions and misconceptions and follows the latest guidance from the World Health Organization (WHO).
Our team’s advocacy for and work with health care workers has been featured in a range of journals and news media, including:



