How we save lives / Epidemic prevention / Epidemic-Ready Primary Health Care
Epidemic-Ready Primary Health Care
Enabling primary health care systems to prevent, detect, and respond to outbreaks while maintaining essential health services.

Epidemics start and end in communities, making primary health care the first point of contact for individuals seeking care—and therefore vital for epidemic preparedness and response. The COVID-19 pandemic placed immense pressure on primary health care systems globally, revealing critical gaps in their readiness and capacity, and underscoring the urgent need for more robust and resilient primary health care systems capable of managing future health crises.
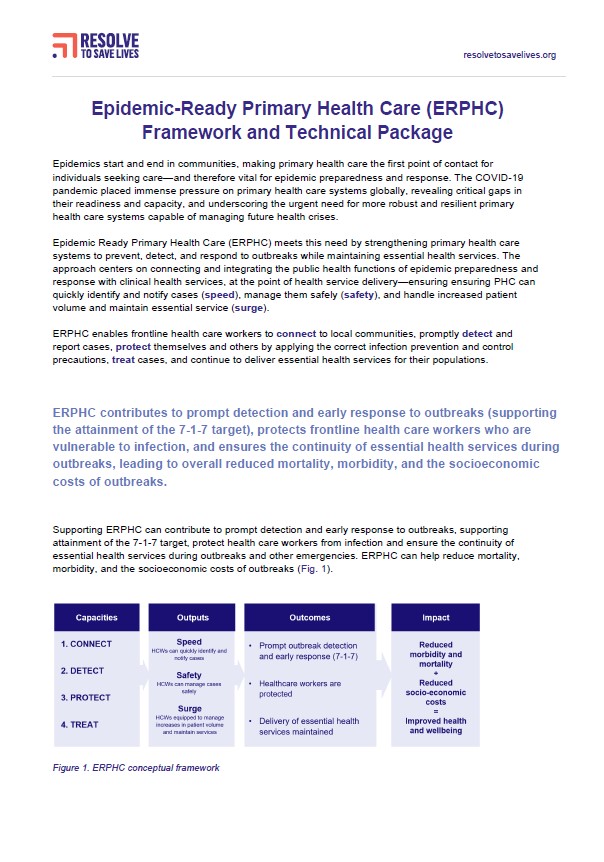
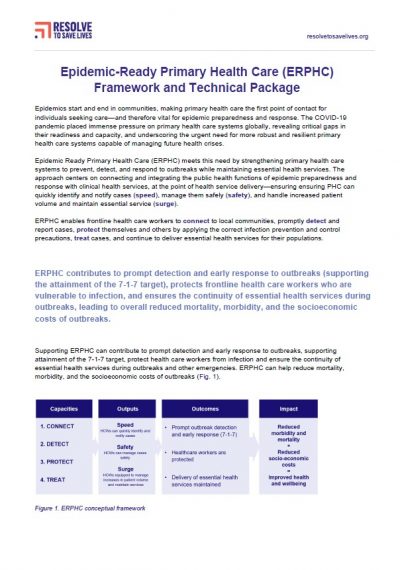
Epidemic Ready Primary Health Care (ERPHC) meets this need by strengthening primary health care systems to prevent, detect, and respond to outbreaks while maintaining essential health services. The approach centers on connecting and integrating the public health functions of epidemic preparedness and response, with clinical health services, at the point of health service delivery. ERPHC enables frontline health care workers to connect to local communities, promptly detect and report cases, protect themselves and others by applying the correct infection prevention and control precautions, treat cases, and continue to deliver essential health services for their populations.

ERPHC contributes to prompt detection and early response to outbreaks (supporting the attainment of the 7-1-7 target), protects frontline health care workers who are vulnerable to infection, and ensures the continuity of essential health services during outbreaks, leading to overall reduced mortality, morbidity, and the socioeconomic costs of outbreaks.
How We Do It
We’re implementing ERPHC with partners at 766 primary health facilities across Ethiopia, Nigeria, Sierra Leone and Uganda, which includes:
Continuous capacity strengthening through regular mentorship to build the knowledge, skills and confidence of health care workers to detect, protect and treat.
Just-in-time training to ensure health care workers have access to update information during times of increased risk. Delivered through our innovative mobile phone-based training package Clinical Integrated Disease Surveillance and Response (cIDSR).
Strengthening public health emergency management approaches at the health facility and subnational level to ensure the continuity of essential health services in the event of a health threat.
Regular assessment of capacities and use of data to inform action planning and performance improvements across levels of the health system.
Improving bidirectional communication and coordination between primary health facilities and public health authorities at subnational level to facilitate rapid detection, notification and response.
Ensuring a safe and protected health workforce, and safe health service delivery through strengthening national infection prevention and control programs and advocacy for increased domestic financing.
How we work
We’re implementing ERPHC with partners at 766 primary health facilities across Ethiopia, Nigeria, Sierra Leone and Uganda, which includes:
Continuous capacity strengthening through regular mentorship to build the knowledge, skills and confidence of health care workers to detect, protect and treat.
Strengthening public health emergency management approaches at the health facility and subnational level to ensure the continuity of essential health services in the event of a health threat.
Just-in-time training to ensure health care workers have access to update information during times of increased risk. Delivered through our innovative mobile phone-based training package Clinical Integrated Disease Surveillance and Response (cIDSR).
Regular assessment of capacities and use of data to inform action planning and performance improvements across levels of the health system.
Improving bidirectional communication and coordination between primary health facilities and public health authorities at subnational level to facilitate rapid detection, notification and response.
Ensuring a safe and protected health workforce, and safe health service delivery through strengthening national infection prevention and control programs and advocacy for increased domestic financing.