How we save lives / Healthier food / Salt reduction / Sodium reduction framework
Sodium reduction framework
This framework outlines the recommended components of a comprehensive dietary sodium reduction program, intended for governments and their partners. The framework also provides links to existing implementation tools, examples of successful programs and policies, and other resources.
You’ve been redirected. LINKScommunity.org is now part of resolvetosavelives.org.
- Introduction
- Governance
-
Surveillance
- Surveillance, monitoring & evaluation plans
-
Collect sodium indicator data
- Establish mean daily sodium intake
- Establish the main sources of dietary sodium
- Sodium content in key packaged food categories
- Establish the levels of iodine fortification and intake
- Assess public knowledge, attitudes and practices (KAP)
- Innovative methods: household budget surveys to assess sodium intake and sources
- Program transparency and accountability
- Regular program review
- Packaged foods
- Food prepared outside the home
- Sodium added in the home
- Appendices and Acknowledgements
Introduction
This framework summarizes the recommended components of a comprehensive dietary sodium reduction program, and provides links to existing implementation tools, examples of successful programs and other resources.
It is designed to be used by governments and their partners in the planning, development and revision of dietary sodium reduction programs. It can also be used to standardize evaluation and review of these programs.
In some cases, as cited in this framework, sodium reduction is addressed through a stand-alone national strategy or program; however, sodium reduction can also be integrated into a broader noncommunicable disease or nutrition strategy. The components of this framework are relevant to both approaches. Cities and regions may also be able implement many of the strategies included in this framework and can work to complement national action.
The framework is organized into five major categories that make up a comprehensive sodium reduction program:
- Governance
- Surveillance
- Interventions for packaged foods
- Interventions for food prepared outside the home (i.e., restaurants, cafeterias)
- Interventions for sodium added at home (i.e., at the table and in cooking)
Several high-priority strategies are outlined for each type of intervention. In some cases, innovative or incompletely tested strategies are listed, particularly in areas where existing solutions are limited, evidence is still emerging, or research on impact has been mixed.
For each component of the framework, a list of resources is provided to guide readers in implementing the strategies. The resources are divided into 1) implementation tools: practical guides or toolkits, 2) other resources: scientific literature, background documents, relevant global guidance, etc., and 3) examples: real world case studies from cities and countries that have implemented these strategies in their local context. The resources and examples provided are not meant to be used as a comprehensive guide but aim to offer users suggestions for further reading on each topic. The resources are limited to resources published in English language.
The framework will be reviewed and updated over time; new resources and examples will be added periodically. Here you’ll find a brief survey where you can submit additional resources and suggestions.
This document is accompanied by a checklist and monitoring tool, found in Appendix 1.
Governance
A systematic and coordinated national strategy is the best way to make meaningful reductions in sodium consumption across the population. This section outlines the key steps required to develop and lead a strategic plan for sodium reduction, engage key stakeholders and decision-makers, and minimize conflicts of interest.
Develop a comprehensive strategic plan
A strategic plan describes the approach the government and other stakeholders will take to lower dietary sodium. It should include: (1) vision and objectives, (2) main interventions and/or policies and their timelines, (3) communications plan, (4) monitoring and evaluation plan, and (5) key stakeholders (for more on stakeholders see Section 1.3).
Other aspects that may be included are an assessment of the political landscape and how different stakeholders will support the objectives. Ideally, the strategy is based on ‘SHAKE’, the World Health Organization (WHO) technical package to support population reduction in dietary sodium and/or regional WHO office strategies. The Pan American Health Organization and the Regional Office for Europe have regional packages/toolkits for salt reduction relevant to strategic planning.
While other countries’ strategies can be used as a model, countries should take into account the unique diets of their population, major sources of dietary sodium, and opportunities and challenges for reducing dietary sodium. The strategic plan should include an overall cost estimate and, ideally, costs per major intervention. The dietary sodium strategy can stand alone or be integrated into a broader noncommunicable disease or nutrition strategy. If dietary sodium reduction is part of a broader strategy, there need to be sufficient resources and priority allocated to successfully implement the sodium reduction-specific interventions.
Regardless of the approach, a successful strategy contains specific interventions to reduce sodium among the country’s primary dietary sources of sodium, whether it comes from packaged foods, food eaten outside the home (e.g., restaurants, canteens, street food), and/or food prepared and eaten in the home.
Successful strategies are usually multi-component approaches that combine a variety of policy measures and behavior change interventions along with a strong monitoring and evaluation component. Examples of comprehensive approaches include the United Kingdom’s salt reduction program as well as the Shandong-Ministry of Health Action on Salt and Hypertension (SMASH) program (He 2014, Xu 2020).
As part of strategic plan development, governments will need to understand the existing landscape, set goals, outline operational and organizational details, and assess costs and benefits. Some countries have formed sodium reduction working groups and/or advisory group to oversee the strategic plan. Further elaborations on these topics are provided in the following sub-sections 1A – 1D.
Implementation tools
World Health Organization. The SHAKE technical package for salt reduction. 2016.
Pan American Health Organization. Salt-Smart Americas: A Guide for Country-Level Action 2013.
Johns Hopkins University. Online Course on Global Sodium Reduction Strategies.
Other resources
Nourishing Database: World Cancer Research Fund International.
Examples
United Kingdom: He FJ et al. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens 2014;28:345-35
South Korea: Park H-K, Lee Y, Kang B-W, et al. Progress on sodium reduction in South Korea. BMJ Global Health 2020;5:e002028.
Conduct a situational analysis (e.g., strengths, weaknesses, opportunities, and threats (SWOT) analysis)
A strategic plan describes the approach the government and other stakeholders will take to lower dietary sodium. It should include: (1) vision and objectives, (2) main interventions and/or policies and their timelines, (3) communications plan, (4) monitoring and evaluation plan, and (5) key stakeholders (for more on stakeholders see Section 1.3).
Other aspects that may be included are an assessment of the political landscape and how different stakeholders will support the objectives. Ideally, the strategy is based on ‘SHAKE’, the World Health Organization (WHO) technical package to support population reduction in dietary sodium and/or regional WHO office strategies. The Pan American Health Organization and the Regional Office for Europe have regional packages/toolkits for salt reduction relevant to strategic planning.
While other countries’ strategies can be used as a model, countries should take into account the unique diets of their population, major sources of dietary sodium, and opportunities and challenges for reducing dietary sodium. The strategic plan should include an overall cost estimate and, ideally, costs per major intervention. The dietary sodium strategy can stand alone or be integrated into a broader noncommunicable disease or nutrition strategy. If dietary sodium reduction is part of a broader strategy, there need to be sufficient resources and priority allocated to successfully implement the sodium reduction-specific interventions.
Regardless of the approach, a successful strategy contains specific interventions to reduce sodium among the country’s primary dietary sources of sodium, whether it comes from packaged foods, food eaten outside the home (e.g., restaurants, canteens, street food), and/or food prepared and eaten in the home.
Successful strategies are usually multi-component approaches that combine a variety of policy measures and behavior change interventions along with a strong monitoring and evaluation component. Examples of comprehensive approaches include the United Kingdom’s salt reduction program as well as the Shandong-Ministry of Health Action on Salt and Hypertension (SMASH) program (He 2014, Xu 2020).
As part of strategic plan development, governments will need to understand the existing landscape, set goals, outline operational and organizational details, and assess costs and benefits. Some countries have formed sodium reduction working groups and/or advisory group to oversee the strategic plan. Further elaborations on these topics are provided in the following sub-sections 1A – 1D.
Implementation tools
World Health Organization. The SHAKE technical package for salt reduction. 2016.
Pan American Health Organization. Salt-Smart Americas: A Guide for Country-Level Action 2013.
Johns Hopkins University. Online Course on Global Sodium Reduction Strategies.
Other resources
Nourishing Database: World Cancer Research Fund International.
Examples
United Kingdom: He FJ et al. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens 2014;28:345-35.
South Korea: Park H-K, Lee Y, Kang B-W, et al. Progress on sodium reduction in South Korea. BMJ Global Health 2020;5:e002028.
Establish and demonstrate the potential benefits of dietary sodium reduction, including cost-effectiveness
Sodium reduction strategies save lives and are cost-effective. Asaria et al. estimated that in low- and middle-income countries (LMICs) a 15% reduction in dietary sodium intake over ten years would prevent 8.4 million deaths (Asaria 2007) and cost only $0.04 to 0.32 per person. At the global level, numerous analyses have found that millions of lives can be saved by dietary sodium reduction (Kontis 2019); there are many country-specific cost-effectiveness studies, which can be enormously useful for securing political buy-in and resources. For example, cost-effectiveness data showing a potential 78-to-1 return on investment in South Korea was critical to winning support for the country’s salt reduction program (Park 2020). In the absence of a local study, countries can use tools such as the Global Burden of Disease to estimate how many lives are lost to high sodium intake.
Set short, mid- and long-term sodium intake goals
Establish long-term and feasible mid-term goals for sodium intake, consistent with the WHO goal of adults consuming less than 2,000 mg sodium/day and the commitments made by many countries to reduce sodium intake by 30% by 2025, following the 66th World Health Assembly in 2013. Defined public goals and timelines will help guide program activities, assess progress and enhance accountability.
Acquired taste for sodium, use of sodium as a preservative, changing people’s usual practices in food preparation, length of time to adapt tastes for sodium, as well as eating habits and use of salt alternatives should be considered when creating feasible short (e.g., 2 years, 10% reduction), mid- (e.g., 5 years, 20% reduction) and long-term targets and goals (e.g., 10 years, majority of population consumes less than 2000mg sodium/day). It is recommended to have a mid-term (e.g., 3-5 year) goal that is feasible and based on a national situational analysis (Section 1.1a). Targets and timelines are important for evaluating the progress of the program over time and for assessing the need for revising interventions and policies.
Examples of mid- and long-term program goals
| Location | Short or Mid-term goal | Long-term goal |
| Global | Reduce sodium intake by 30% by 2025 | Maximum adult intake of 2,000 mg/day |
| Vietnam | Reduce the average salt consumption of adults to 7 g/day between 2018 – 2025. | —- |
| Finland | Reduce salt intake by 20% between 2012-2020. |
Max salt intake:
|
| United States National Salt Reduction Initiative* |
Reduce population sodium intake by 20%, through a reduction in sodium in US packaged and restaurant foods by 25% by from 2009 to 2014 | Maximum limit of 2,300 mg/day |
*This program is a partnership of organizations and health authorities from across the United States, convened by the New York City Health Department, that set voluntary salt reduction targets
Other resources
World Health Organization. Guideline: Sodium intake for adults and children. 2012.
Examples
Vietnam:
South Africa:
Finland:
Israel:
Ministry of Health of Israel. The National Sodium Reduction Program.
United States:
Establish an operational plan with organizational structure and budget
The findings of the situational analysis (Section 1a) can be used to determine the most appropriate interventions and timelines to meet the established goals (Section 1.1c). Interventions that address the most prominent sodium sources should be included (see Sections 3-5 for potential interventions). Where these are unknown, surveillance activities to determine the main sources of sodium (Section 2.2b) should be conducted before selecting specific interventions.
It may also be helpful to review examples of existing sodium reduction interventions from countries around the world. A few organizations provide regularly updated databases or websites that track country examples of sodium reduction policies and interventions. These include the World Cancer Research Fund International’s NOURISHING Database, and the World Action on Salt, Sugar, and Health’s (WASSH) website.
Based on the strategic plan (Section 1.1), the operational plan assigns specific tasks and timelines for reducing dietary sodium to various stakeholders, defines leadership, and establishes accountability. The operational plan should create a structure to optimize implementation and establish a timeline for regular program review. The structure should facilitate smooth long-term interactions of the various stakeholders, linking the people and organizations that need to work together or who have interdependent work to achieve the short, mid- and long-term goals. See Section 1.3 for more detail on stakeholder engagement.
An operational plan should also include the budget necessary to carry out the specific activities in the plan. Costs could include: baseline and ongoing data collection on sodium intake, sodium sources, and sodium levels in foods; public education campaigns; policy development and implementation; human resources; establishing a working group or network, etc.
Implementation tools
World Health Organization: The One Health Tool for Costing Interventions.
Other resources
World Cancer Research Fund International. NOURISHING Database.
Design and conduct an advocacy strategy
Advocacy—activities to support and influence relevant decision-makers to take the necessary actions to promote a salt reduction strategy—will be critical throughout the design and implementation process. These activities may seek to win general support for salt reduction from the government (including commitments to reduce salt intake in the country and prioritization of salt reduction within the government agenda); it may also aim to convince government officials to support and promote a specific policy that will lead to a reduction in salt intake (e.g., adopting salt targets for packaged food, front-of-pack labeling, etc.)
Advocacy is frequently led by civil society groups or other non-profit or academic institutions. Involvement from these groups, and the constituencies they represent, expands the scale and diversity of support for sodium reduction measures; their visible backing for sodium reduction policies can counter opposition from industry and support government stakeholders to take action. Advocacy may also be conducted within the government itself; program leaders may need to convince other officials in order to obtain buy-in within the Ministry of Health; the Ministry of Health may need to obtain buy-in from other agencies such as Ministries of Trade or Finance that are traditionally less focused on health outcomes.
Before designing an advocacy strategy, ensure there is a clear definition of specific goals for sodium reduction (See Section 1.1c), and outline the changes that need to occur for the salt reduction strategy to move forward (See Section 1.1d). Once goals are defined, review findings from the situational analysis (Section 1.1a) to better understand the political and social contexts and identify opportunities as well as threats (e.g., SWOT analysis) for getting sodium reduction onto the current public health agenda, if it is not yet a priority. Also determine what tools and resources are available (e.g., existing data, previous sodium reduction experience and lessons learned in-country or from other countries, financial resources). In most cases, current data on sodium intake, sources, and/or content of foods is important for bringing sodium reduction into the public agenda and convincing stakeholders to take action. Identify key research gaps (refer to the situational analysis) and determine methods and actors/groups to fill these gaps.
Next, build a coalition or network of organizations interested in salt reduction or its related policies. This should start with a stakeholder analysis that examines various actors’ potential roles, level of support (or opposition), and power/influence to determine who to involve to make progress on each goal. Once allies (government bodies, civil society, NGOs, researchers, etc.) are identified and incorporated into the network, the network can meet to agree on common actions (media or political actions), amplify advocacy messages, and ensure a coherent call to action among diverse groups, such as children’s rights, sustainable food systems groups, obesity prevention organizations. Organizational priorities and agendas will vary, but working to find common long-term goals and to highlight partner achievements can encourage collaborative partnerships.
Finally, determine the target audience of the advocacy strategy. This should also derive from the results of the stakeholder analysis, in particular who has the power to make the necessary changes to achieve the identified goals (it may be a different decision-maker or group of decision-makers for each goal). Target audiences often include ministries of health, education, agriculture, and finance, food and drug administrations, and legislators.
Effective advocacy activities take into account what matters to the target audience and tailor arguments to appeal to that audience. Some audiences may find information about the negative health impacts of sodium and the health benefits of policy action compelling; others may find information about cost-effectiveness persuasive. For some decision makers, public and/or media support for the issue may also be critical (especially in the face of industry opposition). Also, consider how sodium reduction may support other policy goals, such as improving children’s health, providing nutritious school food, or supporting local agriculture. In general, it is important to anticipate and address potential concerns from stakeholders and build arguments to address them.
Once you have the building blocks in place, a comprehensive advocacy strategy can be created.This strategy can include many forms of advocacy: strong advocacy efforts include multiple complementary activities.
Advocacy activities commonly conducted by civil society and other groups include:
- Providing background research, fact sheets or policy briefs to decision-makers
- Arranging in-person meetings, phone calls, briefings or workshops with government stakeholders
- Testifying at hearings or presenting at conferences on the health harms of excess sodium and existing successful models in other countries/cities
- Generating relevant local data (e.g., data on sodium content of commonly consumed packaged food products, etc.) and designing advocacy material to inform decision-makers and/or the public about relevant data
- Conducting public awareness campaigns to build public support (using paid mass media, social media, and other channels to reach the public and other stakeholders)
- Contact journalists and/or provide journalist trainings to raise awareness about the importance of salt reduction and advocate for specific action where relevant
- Pursuing earned media coverage (e.g., newspaper or television mentions, placement of op eds in support of sodium reduction strategies)
- Identifying champions that may help get the issue into the public agenda
Advocacy activities commonly conducted by government organizations include:
- Convening workshops and presenting evidence on the need for and benefits of sodium reduction
- Sharing progress reports, publishing press releases, or participating in multi-sectoral mid-term reviews with policymakers to highlight the impact of sodium reduction interventions that are underway (progress reviews also provide an opportunity to address concerns or challenges identified during policy implementation)
Implementation tools
Global Health Advocacy Incubator. Advocacy Tools. Political Mapping tool. (free registration required)
Other resources
Examples
Engage stakeholders
Throughout the process of developing and implementing a national sodium reduction strategy, numerous types of stakeholders will be engaged (see Section 1.3c for examples). This section describes key steps to identifying stakeholders through a stakeholder analysis, engaging stakeholders, and building support among important stakeholder individuals and groups.
Set the agenda
To set the agenda and garner key stakeholders and decision makers’ support for implementing a sodium reduction strategy, a fact sheet and call to action (e.g., Campbell 2016) developed by supportive organizations and individuals can be helpful. The fact sheet should emphasize the current levels of sodium intake, the high rates of premature death and disability caused by high dietary sodium and should be tailored to the specific country using available data, such as national-level data from the Global Burden of Disease. The WHO Sodium Country Score Card, which tracks countries’ progress in implementing legislative and other measures to reduce dietary intake of sodium, can help countries review progress identify gaps, and compare with other countries. Health economic analyses can play a critical role in winning political support given the high returns on investment and cost savings from dietary sodium reduction programs (Section 1.1b). The fact sheet can also provide examples of successful salt reduction policies and interventions.
Implementation tools
Other resources
World Health Organization. The SHAKE technical package for salt reduction. 2016.
Examples
Establish decisionmaker support
Visible, public leadership by a senior government official, such as a Minister of Health, features in many successful dietary sodium strategies. The program needs strong governmental agency secretariat support and budget to provide resources (e.g., financial, staffing) to develop and implement key policies, monitor and evaluate the program and support long-term stakeholder engagement.
Identify and engage key stakeholders
A stakeholder analysis should be conducted to identify the key groups and individuals to engage. Key stakeholders come from many sectors, including government, non-governmental organizations, civil society organizations, academia, media, and the food industry. Stakeholders have different roles to play and should have different levels of influence on the process. The operational plan described in Section 1.1d can outline the key roles and responsibilities of the stakeholders.
Strong government commitment and oversight is needed for success. Ideally, there should be involvement from multiple government departments, including those responsible for nutrition and food regulations, non-communicable disease prevention, surveillance, food procurement, trade, and marketing, advertising, and broadcasting regulations. Nutritionists, dietitians, and other nutrition-specific program experts will also be useful to engage.
Civil society organizations can be important champions of the work. They can help to expand the scale and diversity of support for sodium reduction activities and keep the pressure on government to act. In many countries, civil society may formally support and assist the government with drafting, reviewing or providing comments, and monitoring policies. Key types of organizations to involve include health advocates (e.g., heart or kidney foundations/associations, consumer protection associations), public health and medical associations (e.g., cardiovascular societies, nutrition societies, family physicians, nurses, dietitians), academics (e.g., epidemiologists, nutritional scientists), and education professionals (e.g., culinary schools, health staff in schools). Engaging global organizations may be helpful to gain insight from ongoing sodium reduction programs in other jurisdictions. Well-known role models (e.g., athletes, celebrities, entrepreneurs, chefs) may also play a role in raising awareness and building support for salt reduction programs and policies.
While the food industry is a stakeholder in many sodium reduction policies and should have a structured opportunity for input on specific policies that impact the industry, this process needs to be transparent and governed by a strong conflict of interest policy (See Section 1.4).
See Section 1.3 for further details on stakeholder advocacy.
Implementation tools
World Health Organization. Stakeholder Analysis.World Health Organization. Accelerating Nutrition Improvements (ANI) Mapping of stakeholders and nutrition actions in three scaling-up countries in sub-Saharan Africa. Report of a meeting. 2014.
Other resources
Examples
Pan American Health Organization: PAHO. Salt-Smart Americas: A Guide for Country-Level Action. 2013.
South Africa: Webster J. et al. South Africa’s salt reduction strategy: Are we on track, and what lies ahead? S. Afr. med. j. 2017; 107.1. (Report of a stakeholder meeting in South Africa)
Victoria, Australia: Rosewarne E et al. Stakeholder perspectives on the effectiveness of the Victorian Salt Reduction Partnership: a qualitative study. BMC Nutr 7, 12 (2021).
Counter scientific opposition
In some cases, there may be arguments against sodium reduction by members of the scientific community or other stakeholders. It is important to note that scientific controversy has been created by a small group of scientists who suggest that low levels of sodium can increase cardiovascular mortality. These arguments are based on observational studies that rely on lower quality methods of measuring sodium intake. Other problems in the literature include reverse causality, lack of rigor in research, conflicts of interest and commercial bias (Cobb 2020, Campbell 2021). Rigorous reviews of the evidence for sodium reduction, such as those completed by the National Academies of Medicine or the European Food Safety Authority, have consistently concluded that sodium intake should be limited to 2,000 or 2,300 mg/day to protect cardiovascular health. Stakeholders, especially those from academia, can be involved to counter scientific opposition from other stakeholders using documented high quality, rigorous research from unbiased sources, emphasizing the clear impact of high sodium intake on blood pressure levels and the benefits of sodium reduction on cardiovascular health outcomes.
Other resources
Mitigate conflicts of interest
The food industry is one of the largest in the world (and a dominant industry in many countries); it has long opposed policies and regulations that could impact its profits. Industry associations at both the global and national level represent the commercial interests of the food industry and will likely oppose policies that reduce sodium in their products. The food industry has created and funded organizations to evaluate science from an ‘industry-friendly’ perspective by creating educational programs and hiring scientists and clinicians to represent industry interests and often funds their meetings and presentations (Campbell 2021). The source of funding may not be disclosed or can be misrepresented (by using a third-party organization, such as the International Life Sciences Institute (ILSI), or funding to an academic or health organization).
Creating a structured approach for industry and people with industry ties to comment on a draft policy, without including them in policy development or final decision-making, is strongly recommended. There are several policies and/or regulations that can reduce the impact of conflicts of interest during the policy process.
Best practice is to:
- Define conflicts of interest broadly and comprehensively
- Require written disclosure of financial interests at regular intervals (e.g., annually) by all parties involved
- Include groups acting in the public and public health interest (e.g., academics, civil society, etc.) as part of the policy process
- Develop strategies for mutual accountability and monitoring.
Other resources
The SUN Movement Toolkit for Preventing and Managing Conflicts of Interest. 2014
The New York Times. Jacobs A. A shadowy industry Group Shapes food policy around the world. 2019.
Global Healthy Advocacy Incubator (GHAI) Resources:
Global Health Advocacy Incubator (GHAI). Countering Industry Interference: Industry Watch Resources.
GHAI: Front of Package Labeling – Industry Arguments: Counter Messages and Evidence. August 2021.
Industry Interference Policy Briefs No. 1: Industry Interference in Food Policy.
Surveillance
A comprehensive strategic plan for sodium reduction will require a robust surveillance strategy to monitor key sodium indicators, evaluate progress and impact and optimize the plan over time. Data should be made publicly accessible in order to ensure transparency and hold the government accountable to its goals.
Develop surveillance, monitoring and evaluation plans
A surveillance, monitoring and evaluation plan should establish ways to measure progress toward the goals outlined in the strategic plan (Section 1.1), including:
- Baseline and follow-up measurements of average population sodium intake
- Major sources of dietary sodium and the levels of sodium in foods targeted by the program
- Monitoring of interventions, which can include process indicators to monitor whether actions have been implemented in the timeframe outlined in the operational plan
- Interim indicators, such as the knowledge, attitudes, and practices (KAP) of segments of the public, which can contribute to monitoring program progress, barriers, or facilitators (see Section 2.2e).
The plan should outline the frequency of measuring key indicators and should include the required budget, the necessary research and laboratory capacity, and the steps required to build capacity if needed. It is ideal to assess all population indicators in a representative sample with adequate statistical power to examine changes over time and among specific sub populations of interest (e.g., different ethnic populations who may have unique dietary patterns, men vs. women, and key age groups).
Initiatives to reduce dietary sodium can begin while baseline data is being collected, provided the major sources of dietary sodium are known (understanding that the intervention may impact the baseline data).
Surveillance, monitoring, and evaluation plans are often developed and overseen by the sodium reduction advisory or working group; however, in many cases academic institutions or other research groups may be involved. It may be useful to have an independent group conducting surveillance activities. Surveillance of sodium intake and sources of salt can also be built into regularly schedule population surveys, such as WHO STEPS survey or the Demographic and Health Surveys. Additionally, ongoing monitoring and evaluation can be built into existing systems, for example, within health services or food safety systems.
The checklist in Appendix 1 can be used to structure a regular program review
Other resources
World Health Organization. SHAKE the salt habit: The SHAKE technical package for salt reduction. 2016. (See section on: Surveillance: Measure and Monitor Salt Use)
WHO EURO. Accelerating salt reduction in Europe: a country support package to reduce population salt intake in the WHO European Region. 2020. (See sections 2.7 and 3)
Pan American Health Organization. Salt-Smart Americas. A Guide for
Country-Level Action. 2013.
Examples
Collect sodium indicator data
The Surveillance, Monitoring, and Evaluation Plan (Section 2.1) will outline indicators that should be established at baseline and repeatedly measured throughout and after interventions take place. This section describes the key indicators to measure, including mean sodium intake; dietary sources of sodium; sodium content in packaged foods; iodine intake and fortification levels; and knowledge, attitudes, and practices related to sodium.
Establish mean daily sodium intake
Mean dietary sodium provides information on intake relative to the WHO recommended maximum adult intake of 2,000 mg of sodium (5 g salt) per day and sets the baseline for measuring future progress. Assess sodium intake through a nationally representative, adequately powered survey.
Several different methodologies can be used for measuring mean daily sodium intake. While more expensive and labor-intensive than other methods, the most accurate method is to collect complete 24-hour urine samples and analyze them for sodium and creatinine. (Although single 24-hour urine collections are not a reliable indicator of an individual’s usual sodium intake, the method is accurate on a population basis if the urine collections are complete.).
Measurement of sodium and creatinine using spot urine samples can be used to estimate average population 24-hour sodium intake. This method is used as part of the WHO STEPS survey and is less expensive and technically much easier than 24-hour urine collection. While it appears to be an acceptable way to assess the average population sodium intake at a single time point, using spot urine samples to assess change in average population sodium intake over time is considered to be less reliable (though research is still ongoing). Spot urine samples also underestimate the distribution of sodium intake. Ideally, if using spot urine samples, there should be a validation sub-sample where 24-hour urine samples are collected.
Dietary recall surveys (e.g., one or more 24-hour recalls) are another option for measuring sodium intake. Validity is highly dependent on the recall ability of the respondents, completeness and accuracy of the food database used to support the survey, and it is an unreliable method for assessing sodium added during cooking or at the table. While sodium intake can be significantly underestimated using this method (especially where food databases are less reliable or large proportions of sodium are added at home, in cooking or at the table), one advantage of the dietary recall survey is that it also assesses the dietary sources of sodium and provides information that is valuable for other, complementary nutrition initiatives. In some cases, surveys also quantified sodium intake using food weighing methods (Du 2014).
Implementation tools
PAHO: Protocol for Population Level Sodium Determination in 24‐hour Urine Samples. 2010.
Other resources
World Health Organization. WHO STEPwise approach to surveillance (STEPS). (see link for data collection instruments, user manual, and country reports)
Examples
Establish the main sources of dietary sodium
Dietary sodium is typically consumed from three distinct sources: sodium added to packaged food during manufacturing, sodium added to food consumed outside the home (e.g., restaurants, street food vendors, cafeterias/canteens), and discretionary sources (sodium added in the home, either during cooking or while eating). The main dietary sources of sodium are usually established by dietary recall surveys or food frequency questionnaires (FFQ). The validity of the survey results is highly dependent on the recall ability of the respondents and the accuracy and completeness of the sodium content of the foods in the database used to support the survey. It is important to have data for the sodium content in targeted primary sources of sodium in order to track reductions over time (in addition to broader data on population sodium intake). Developing and updating a database to track the sodium content of foods is important for tracking changes that may occur during the intervention. If the intervention is successful, there may also be changes in the main dietary sources of sodium.
If it is not possible to pinpoint the main dietary sources of sodium, understanding the main components of the diet (regardless of the sodium content) can help plan and prioritize interventions.
Implementation tools
WHO/PAHO: A review of methods to determine the main sources of salt in the diet. 2010.
Examples
China, Japan, UK, U.S.: Anderson CA, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. JADA 2010 May 1;110(5):736-45.
Identify the sodium content in key packaged food categories
Many of the well-defined, evidenced-based policies to reduce sodium intake focus on packaged foods. A crucial starting point for these policies is to establish a database including key categories of packaged foods and their sodium levels. The easiest way to build this type of database is to use the sodium content from nutrition labels. Appendix 3 provides guidance on developing a food database via visits to food retail stores. In some settings, most of the data can be collected efficiently from online sources, and commercial groups may sell data on the nutrient content of packaged foods. Various technologies have been developed to assist collection of packaged food label data, such as applications that allow for simpler in-person data collection (e.g., FLIP, FoodSwitch), web-scraping techniques (e.g., foodDB), or crowd-sourcing (e.g., FoodSwitch).
While the Food and Agriculture Organization and WHO’s Codex Alimentarius (“Codex”) recommends that sodium be required on packaged food nutrient declarations, many countries still do not require it. See Section 3.2a for specific recommendations on mandatory nutrient declaration labeling. In addition to collecting label data, it may be necessary to measure the sodium level of selected foods for monitoring; in some countries, labeled nutrient content can be inaccurate even if labeling is required. Government food authorities can also create a national database of packaged foods by making it mandatory for food industry to submit nutritional content (including sodium) of packaged foods when applying for product registration.
Implementation tools
Resolve to Save Lives. Appendix 3. Instructions for developing a food database.
Other resources
FAO and WHO. International food standards (FAO/WHO Codex Alimentarius).
The George Institute for Global Health. FoodSwitch mobile application. (See for data collection tool)
The Global Food Monitoring Initiative. (See for sample protocols)
Examples
Latin America/Caribbean: Arcand J et al. Sodium Levels in Packaged Foods Sold in 14 Latin American and Caribbean Countries: A Food Label. Nutrients. 2019;11, 369.
Establish the levels of iodine fortification and intake
Once a major global public health concern, iodine deficiency has been largely overcome in many countries by iodizing salt. The levels of iodine added to salt should be based on sodium intake in the population; more iodine can be added as sodium intake falls, allowing for optimum intake of both nutrients. Iodine fortification and sodium reduction programs are thus mutually compatible and should be coordinated wherever possible in terms of both advocacy and communication (to policymakers, the food industry and the public) and to program surveillance and evaluation.
Iodine intake can be monitored along with sodium, with particular attention to the populations most vulnerable to iodine deficiency: children and pregnant women.Iodine is typically assessed using spot urine samples but, like sodium, can be more accurately measured using complete 24-hour urine samples.
Other resources
Examples
China:
Netherlands:
South Africa, Ghana:
Assess public knowledge, attitudes and practices (KAP)
Assessing the public’s knowledge, attitudes and practices (KAP) relating to dietary sodium can help in the design and monitoring of behavior change and education programs and provides a baseline of the public’s receptivity to and support of potential policy interventions. The result of repeated KAP surveys can be used to track the effectiveness of mass media campaigns, educational interventions and policy changes. However, monitoring changes in practice through KAP indicators cannot replace a quantitative assessment of sodium intake; many projects have seen changes in KAP survey indicators without changes to sodium intake.
KAP surveys can also be designed to assess the food industry’s knowledge, willingness and intention to change, the support or challenges from the health and scientific sector and from policymakers.
Implementation tools
Other resources
Examples
South Africa, Ghana: Menyanu E et al. Salt Use Behaviours of Ghanaians and South Africans: A Comparative Study of Knowledge, Attitudes and Practices. Nutrients 2017, 9, 939.
Ethiopia: Survey on salt consumption knowledge, attitudes and practices and blood pressure in Ethiopia.
Innovative methods: household budget surveys to assess sodium intake and sources
A small number of countries (Brazil, Poland, Slovenia, and Costa Rica) have used Household Budget Surveys (HBS) to estimate average sodium consumption and major dietary sources of sodium. The method is rapid and inexpensive, with most countries collecting data through HBS every 4-5 years. There is inadequate research at this time to assess the generalizability or reliability of using this approach.
Program transparency and accountability
Once established, indicators for reducing dietary sodium should be made easily and publicly accessible to encourage transparency and accountability for the program. Making data available to the health and scientific community for analysis and dissemination applies pressure on the food sector to meet sodium targets in their products and on program leaders to meet overall program goals. Consumer protection groups can play an important role in ensuring accountability through communications with the public.
Other resources
Examples
Canada:
Health Canada’s Trans Fat Monitoring Program (not sodium, but excellent example).
United States:
Regular program review
Sodium program operational plans (Section 1.1d) need to be reviewed and adjusted to account for lessons learned. Regular program review (e.g., annually) by the working group or other body identified in the strategic plan should assess progress towards targets and also take into account overall trends in dietary intake and sources.
Interventions for packaged foods
Addressing sodium consumption from packaged foods is an important component of a salt reduction strategy where packaged food consumption is high or growing. Regulatory approaches are typically most effective for reducing sodium in packaged foods (Hyseni 2017). Multiple strategies exist for reducing sodium intake from packaged foods, including setting targets to lower the sodium content in packaged foods, mandating accurate nutrition labels, fiscal policies (taxation of high-sodium or junk foods/HFSS foods (high fat, sugar, salt)) and subsidies to incentivize consumers to make healthier choices), and limits on what foods can be marketed/advertised to children. One strategy to lower the sodium content of packaged foods without altering taste is the partial substitution of salt with low-sodium salt. Low-sodium salt is discussed further in Section 5.2.
Nutrient profiling models
Nutrient profile models classify foods according to their nutritional quality. Government-led nutrient profiling is critical to the implementation of nutrition policies such as front-of-pack labels, fiscal policies and marketing regulations on unhealthy foods. Industry-developed labeling programs that rely on nutrient thresholds are part of marketing a company’s products and are not appropriate for public health interventions. Nutrient profiles specify thresholds for each nutrient (most include only harmful nutrients such as sodium, sugar and saturated fat). Nutrient thresholds may or may not vary by category. Some nutrient profile models focus on identifying foods that people should avoid, some on identifying better-for-you foods, and others on creating a system to rate foods based on overall healthfulness. The type of nutrient profile will depend on how the model will be used. For instance, in marketing restrictions, a nutrient profile model establishes thresholds above which products cannot be marketed to children, whereas certain front-of-package labels classify foods into multiple categories (e.g. red, yellow or green for traffic light labels) and therefore require a nutrient profile model that provides multiple thresholds.
Countries can often utilize existing nutrient profile models from another country with effective nutrition policies, as long as the model can be adapted to fit the new context based on the food categories commonly consumed. The WHO has developed regional nutrient profile models, mostly for restricting marketing of unhealthy food to children. These may be adapted for other policies as well (see the resources section below for links to the WHO nutrient profile models).
Other resources
Global Health Advocacy Incubator. Nutrient Profile Models Position Paper. 2024
WHO Nutrient Profiling: Report of a WHO/IASO Technical Meeting
WHO regional nutrient profile models:
WHO Nutrient profile model for the WHO African Region
Pan American Health Organization nutrient profile model
WHO Nutrient profile model for the marketing of food and non-alcoholic beverages to children in the
WHO Eastern Mediterranean Region
WHO Regional Office for Europe nutrient profile model
WHO nutrient profile model for South-East Asia Region
WHO nutrient profile model for the Western Pacific Region
Examples
Bogotá, Colombia: Mora-Plazas M, et al. Nutrition Quality of Packaged Foods in Bogotá, Colombia: A Comparison of Two Nutrient Profile Models. Nutrients. 2019 May 4;11(5):1011.
* Interventions identified as WHO ‘best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases.
^ Interventions identified as Recommended priority actions in: Ide N et al. Priority actions to Advance Population Sodium Reduction. Nutrients 2020.
Labeling interventions for packaged foods
Labeling of packaged foods for sodium content (and other nutrients with critical health impact) provides consumers with information so they can avoid less healthy products and select healthier products; labeling also stimulates industry reformulation and new product development.
Mandatory nutrient declaration labels*
At a minimum, national regulations for packaged food labels should require a list of ingredients in descending order of weight and a nutrient declaration including calories, sodium, potassium, sugar, trans fat, and saturated fat (accurate to within 20%). Independent monitoring of the accuracy of labels is important. According to CODEX guidelines, information on nutrient content should be numerical; for example, expressed in g per 100 g or per 100 ml or per package if the package contains only a single portion. Appropriate back of package labeling alone will not lead to lower sodium intake or lower sodium content of packaged foods but is foundational to other packaged food interventions.
Other resources
FAO and WHO. Food Labelling. Fifth Edition. 2007. (See section: ‘Guidelines on Nutrition Labelling CAC/GL 2-1985′)
Examples
United States: US FDA. How to Understand and Use the Nutrition Facts Label.
Regulations restricting health claims on food packages
Food manufacturers will often put a health or quality claim on food packages or other marketing materials; these claims may be regulated by the government. CODEX guidelines offer the following definitions for claims on sodium content:
- Low sodium = not more than 0.12 g per 100 g
- Very low sodium = 0.04 g per 100 g
- Sodium free = 0.005 g per 100g
However, even when regulated, many health claims can be difficult for consumers to understand and may create a “health halo effect,” misleading consumers to believe a product is healthy when it is not. For example, a claim on a package that a food contains “low sodium” may lead a consumer to believe it is healthy when in fact it may be high in saturated fat or sugar. At minimum, health claims should not be allowed on packages of food that contain high quantities of sodium, sugar or saturated fat (or that are otherwise unhealthy based on the government’s nutrient profile).
Other resources
FAO and WHO. Food Labelling. Fifth Edition. 2007. (See section: ‘Guidelines for Use of Nutrition and Health Claims CAC/GL 23-1997′)
Examples
Global: NOURISHING: Nutrition label standards and regulations on the use of claims and implied claims on food. (See sub-sections on “rules on nutrient claims”)
Front-of-package labeling regulations
More recently, some governments have required that manufacturers place interpretive labels on the front of food packages to help consumers choose healthier products or avoid unhealthy products. A variety of front-of-package labeling (FOPL) systems are in use, with some indicating how healthy a food is based on its nutrient profile (e.g., star- or score-based systems) and others showing whether a product contains high amounts of sodium or other nutrients of concern (e.g., warning labels, traffic lights). To date, the only approach to show impact on improved consumer purchasing after policy implementation is a prominent warning label that highlights that a product is high in sodium, saturated fat, and/or sugar (some countries also include trans fat and/or calories). An evaluation of this model in Chile showed a 37% drop in sales for regulated junk foods with “high in sodium” warning labels, along with further reductions for foods high in sugar, saturated fat, and calories.
Implementation tools
Other resources
Examples
Chile:
Pan American Health Organization. Approval of a New Food Act in Chile Process Summary. 2017.
Government-led sodium targets for packaged food*^
Setting targets for salt levels in packaged foods is a WHO “Best Buy” intervention for addressing non-communicable diseases (NCDs). Sodium targets work best when they are government-led and accompanied by robust monitoring and accountability systems. Salt targets can be voluntary or mandatory. The initial phase of United Kingdom’s government-led voluntary targets resulted in a 15% reduction in salt intake and successfully reduced salt in many categories (He 2014); however, many other voluntary programs have been less successful, given that industry has less incentive to reformulate under voluntary programs. Mandatory targets may have a greater impact on the sodium levels in foods than voluntary approaches (Cobiac 2010).
Targets can be set for maximum levels of sodium content by food category and/or for the average levels of sodium by food category. If sales information is available, which is rare, the sales-weighted average can be used to set targets by food category (Institute of Medicine 2010). Maximum levels are easier to develop and monitor and lend themselves better to a regulatory approach; however, because they affect only the foods highest in sodium, they often have less impact on overall sodium consumed and need to be lowered over time.
Ideally, targets cover a majority of packaged foods in a country (e.g., the UK set targets for 84 food groups in 2020). If this is not possible, and certain categories can be identified as the prime sources of sodium intake, targets can be set for a smaller set of categories to start with (e.g., bread, condiments). The targets and timelines for sodium content of food categories are usually revised at defined intervals and reset to lower levels over time while also adding any new food categories that are significant contributors to sodium intake.
Implementation tools
WHO South-East Asia Region Sodium Benchmarks for Packaged Foods. 2024.
Other resources
Examples
Argentina: Government of Argentina. Law 26905. Sodium consumption – maximum values. 2013.
United Kingdom:
United Kingdom salt reduction targets for 2024.
Canada: Canada’s Guidance for the Food Industry on Reducing Sodium in Processed Foods.
Global: NOURISHING Framework. Section I: Improve nutritional quality of the whole food supply.
Restrictions on marketing to children^
Unhealthy food and beverages are often marketed to children. Food marketing can impact a child’s food and drink preferences, eating behavior, and food intake. WHO recommends restricting or prohibiting the marketing of unhealthy foods to children. Marketing restrictions should be robust, clear and evidence-based. The ideal marketing regulation is:
- mandatory
- protects children under the age of 18
- includes all forms of marketing (e.g., social media, in-store, television, radio, internet games, promotions in schools, sponsorship of children’s events, etc.)
- uses a nutrient profile model to decide which products cannot be marketed
To be effective, marketing restrictions cannot only affect programs and activities narrowly targeted at children but should also include marketing for a broader audience often seen by those under 18. Ideally, as in Chile, this should align with packaged food warning labels, food procurement standards for schools and other government institutions.
Marketing restrictions may be imposed more broadly to promote healthy eating for everyone. For example, in 2018, London, England restricted advertising for foods and non-alcoholic drinks high in fat, salt and/or sugar on all public transportation, including railways, buses and taxis (Mayor of London 2018).
Implementation tools
Other resources
World Health Organization. Protecting children from the harmful impact of food marketing: policy brief. 2022 (See the resources in Section 9 for a list of WHO Nutrient Profile Models developed for the restriction of food and non-alcoholic beverage marketing to children.)
Examples
Global: NOURISHING Framework: Restrict food advertising and other forms of commercial promotion.
Chile: Pan American Health Organization. Approval of a New Food Act in Chile Process Summary. 2017.
Fiscal policies
Taxation is a well-established public health approach to reducing consumption of tobacco and alcohol. Taxes on sugar-sweetened beverages have been gaining momentum and have been shown to reduce consumption of sugar when the taxes are substantial; the evidence for other types of food taxes is still being established. A small number of countries, including Mexico, Hungary, Fiji, Tonga, and Saint Vincent and the Grenadines, have instituted junk food taxes or taxes on products that are high in sodium, sugar or saturated fat. These types of taxes may be effective in reducing both the sodium content in food products as well as the amount of high- sodium foods purchased and consumed by the public.
Taxes should be high enough to deter consumption and structured so that substitute products are healthier than taxed products. Taxes to reduce salt intake could either target high-salt foods specifically or junk foods more broadly. Combining taxes with subsidies for healthy foods (e.g., fresh fruits and vegetables) may help offset any burden that taxation may impose on lower-income people who do not change their purchasing patterns (and also increases purchasing of healthy foods).
In addition to taxation, other fiscal policies include:
- Reducing costs of healthy foods by subsidizing fruits and vegetables or other healthy foods, which can also impact purchasing behaviors and potentially reduce dietary sodium
- Tariffs on the import of unhealthy foods
Implementation tools
WHO EURO. Using price policies to promote healthier diets. 2015.
World Cancer Research Fund International.Lessons on implementing a robust sugar sweetened beverage tax. 2018. (Focuses on sugar sweetened beverage taxes, although many lessons can be applied to potential salt or junk food/HFSS taxes)
Other resources
Examples
Innovative/other policies for packaged foods
Innovative or incompletely tested interventions are listed where evidence is still emerging or research on impact has been mixed.
Food based dietary guidelines
Brazil and some other countries are moving towards guidelines that promote fresh or minimally processed foods and discourage consumption of highly processed foods. While these are not specifically targeted at changing packaged foods, they aim to disrupt the global trend toward increasing reliance on packaged foods.
Placement, price and marketing of healthy and unhealthy foods in grocery stores
The “4 Ps” of marketing (product, placement, price, and promotion) are used by food retailers to market foods to consumers and can be used to create an enabling environment for healthier choices. Researchers have found that price discounts, product promotions (e.g., food tastings), and visible/accessible placement are the most effective strategies for increasing sales of healthy foods (Hartmann-Boyce 2018, Moore 2014). While this has been studied extensively, there have been no large-scale public health interventions of this kind to date.
Location of food retailers relative to schools
Some jurisdictions have regulated what kinds of foods can be sold in establishments that are near schools. For example, the India School Children Regulation and the South Korea ‘Green Food Zones’ specify what foods are prohibited for sale and marketing within a designated perimeter of school grounds.
Prohibiting sales of unhealthy food to children
In addition to restricting marketing of unhealthy foods to children, multiple jurisdictions in Mexico have recently developed regulations that restrict the sale of unhealthy food to children unless they are accompanied by a parent. The feasibility and impact on reducing dietary sodium has not yet been assessed.
Other resources
Examples
London, UK: Evening Standard. UK’s first supermarket designed by public health experts launches in Central London
Oaxaca, Mexico: BBC. Mexico obesity: Oaxaca bans sale of junk food to children. 2020.
Interventions for Food prepared outside the home
Sodium intake from food prepared outside the home—such as from canteens, restaurants and street vendors—is increasing in many countries, as people have less time to prepare food at home and more income to spend on prepared food. Reducing sodium in these environments can be challenging, as the industry is often made up of large numbers of lightly regulated (or unregulated) small businesses; however, a number of innovative strategies have been proposed. Additionally, governments can introduce standards for foods the government purchases, serves or sells, impacting large numbers of people and setting an example for the private sector. In some cases, cities or states may have jurisdiction in these environments.
Healthy public food procurement and service policies*^
In many settings, significant amounts of food are purchased with public funds and are served and sold in public institutions (e.g., schools/school meal programs, parks, hospitals, correctional facilities, government office canteens/cafeterias). Establishing and implementing a comprehensive healthy food procurement and service policy for all government agencies increases public access to healthier meals and snacks, with more fresh and less ultra-processed food. A food procurement and service policy sets standards for healthier eating environments, provides internal consistency with a dietary sodium reduction program, and may also prompt the food industry to develop lower sodium products in order to compete for government contracts.
Public food procurement and service policies can be combined with other policies to reduce sodium, such as front-of-package labeling (Section 3.2c) and marketing restrictions (Section 3.4) to create a more effective and comprehensive package of interventions. It can also incorporate other strategies such as the use of low-sodium salt (Section 5.2) and public educational approaches (Section 5.1) to complement implementation of the policy. Further, these policies can be used as a model which can be adopted by private entities to serve or sell healthier, lower-sodium food.
Implementation tools
Other resources
Resolve to Save Lives. Resources for Healthy Public Food Procurement and Service Policies.
U.S. CDC. Healthy Food Environments. 2021.
Examples
Global: NOURISHING Framework. Section I: Improve nutritional quality of the whole food supply.
Global: Resolve to Save Lives. Resources for Healthy Public Food Procurement and Service Policies. (Use filtering feature for “policy examples”)
ACT, Australia: ACT, Australia: ACT Public Sector Healthy Food and Drink Choices Policy. 2016.
New York City, USA:
NYC Health. New York City Food Standards. 2008.
Quezon City, Philippines: Health Public Food Procurement in Quezon City, Philippines, 2020.
Restaurant and street food interventions
Evidence on restaurant or street food interventions is still emerging; few have been evaluated and where they have, the results have been mixed. Some of the strategies outlined below could apply to all restaurants or street vendors (Section 4.21a), while others are limited to chain restaurants (Section 4.2b). Alone, many of the strategies below may have minimal impact; however, that impact could be greatly increased if implemented together with low-sodium salt substitution (Section 5.2). Additionally, consumer-facing education approaches can encourage ordering of low-sodium dishes.
Key interventions for all types of restaurants
Leverage existing packaged food salt reduction strategies to reduce salt in foods purchased by restaurants
Ensuring that salt reduction targets for packaged foods (whether voluntary or mandatory) apply to ingredients purchased by restaurants and street vendors will likely reduce sodium levels in restaurant foods. Additionally, regulations for restaurants could leverage labeling schemes such as front-of-pack warning labels and restaurants could be required to avoid purchasing products with warning labels. While this strategy is untried, it is based on successes setting sodium thresholds for purchased foods in public food procurement policies and also trans fat thresholds for restaurant purchases of packaged foods as part of trans fat restriction policies (Angell 2009).
Other resources
Require that salt shakers and condiments high in sodium be available by request only
Several countries have restricted restaurants from placing salt shakers and high-salt condiments on tables, usually in combination with an education campaign. Customers must request the salt shaker and condiments. Similarly, if restaurants use individual salt packages, these can also be provided only upon request and the size of the package can be reduced (e.g., from 1 g to 0.5 g salt per package) to help encourage reduced consumption.
Examples
Uruguay: NPR. The Salt. Assault on Salt: Uruguay Bans Shakers in Restaurants and Schools. 2015.
Argentina: Argentina Food Law 26.905. Sodium consumption. Maximum Values. Article 5G. 2013.
Require restaurants to make a certain number of menu items with no or low added salt
To enhance customer choice within the restaurant setting, a few jurisdictions require that a certain number (or percentage) of menu items are low-salt or no salt added. Highlighting these items, often in combination with a mass media campaign about the health impact of sodium intake, can provide consumers with important information, particularly outside the chain restaurant environment, where nutrition information is limited. This intervention is likely to mostly benefit customers already motivated to reduce salt intake.
Examples
Montevideo, Uruguay: Devex. Cities and NCDs: Montevideo’s menu for reducing sodium intake. 2018.
Require a sodium warning statement on menus
Cities and countries can put mandatory policies in place requiring a health message about sodium intake and its relationship to health outcomes on menus and/or menu boards. These warning statements are sometimes only required in chain restaurants, where there is also access to nutrition information, and can be used in combination with high-sodium warning icons on specific menu items.
Examples
New York City, USA: Anekwe AV, et al. New York City’s sodium warning regulation: from conception to enforcement. American journal of public health. 2019 Sep 1;109(9):1191-2.
Create targeted education campaigns for restaurant staff and/or chefs
Many restaurant strategies include an educational component for restaurant staff, which can be delivered during mandatory food safety training required to receive a food handler license or specific training opportunities for restaurant chefs. Trainings may include information on the harms of excessive sodium intake, tips on developing new menu items with reduced sodium content, and ways to work with suppliers to source lower-sodium ingredients. Toolkits distributed to restaurants (e.g., Ma 2018) may include recipes, kitchen utensils and a standard measuring spoon.
While this education and training can complement other interventions and target particularly vulnerable communities, it is resource-intensive and may be hard to scale. Other interventions should be used in tandem to ensure the continuity of the sodium-reduction strategy.
Examples
Other resources
Interventions for chain restaurants
Require public disclosure of nutrition information at every point of sale
As a first step, all chain restaurants should be required to publicly disclose nutrition information through a nutrition board/cards for all standard menu items, along with toppings, side dishes, beverages, and promotional items. Information should include all key nutrient information that is often available on packaged food nutrition labels: calories/energy, saturated fat, total fat, trans fat, sodium, sugar, and fiber content, along with ingredients and allergen information.
Public disclosure of nutrition information allows for tracking nutrient content of menu items in chain restaurants, provides consumers information on nutrition and ingredients, and ensures that public health policies can be monitored and enforced. There is a clear need for transparency in chain restaurant nutrition information to enhance industry accountability and government monitoring of nutrition commitments. Public disclosure of nutrition information should include making it available at the point of purchase where consumers are making decisions—in stores and as part of online ordering for pickup or delivery.
Require high-sodium warning icons
Public disclosure of nutrition information requires motivated consumers to check sodium content and understand recommended daily intake limits. At least six policies are in place globally (mostly in North America, Europe, and Hong Kong) that use icons on menus to communicate sodium information to customers, reducing the burden on consumers, and some countries, including the United States and India (to be enforced from January 1, 2022), require calorie labeling on chain menu items. To date, the impact of menu labeling on menu reformulation has been mixed (Alexander 2021), with some studies showing a reduction in the sodium content of menu items and others showing no impact.
Other resources
Examples
New York City, USA: Amaka VA. et al. 2019: New York City’s Sodium Warning Regulation: From Conception to Enforcement American Journal of Public Health. 2019 Sep 1;109(9):1191-2.
Sweden:
Swedish Food Agency. The Keyhole.
Hong Kong: Hong Kong Department of Health. EatSmart Restaurant Star+ Campaign.
Set sodium content limits for menu items
Governments can set thresholds for the total amount of sodium contained in a restaurant menu item. While possible in all types of restaurants, these policies are most feasible for chain restaurants, where ingredient composition is standardized and nutrition information is available. The variation in sodium content that currently exists between restaurant chains in different countries indicates that technical feasibility is not the limiting factor, and substantial reductions could be made that would improve population health (Dunford 2012).To be successful, sodium content limits would likely need to be mandatory.
Examples
Global:
England: Public Health England. Salt reduction targets for 2024. 2020. (See the description on page 4 on the requirements for the out of home food sector to meet certain sodium targets)
Set sodium (and other nutrient) content limits for meals marketed to children
Sodium limits can also be set specifically for meals targeted to children. Standards should reflect the appropriate sodium intake for children and may be combined with other nutrient requirements, such as calorie and/or fat limits and minimum servings of fruits and vegetables. A U.S. study found that the majority of meals ordered for children were not from kids’ menus, so any comprehensive policy designed to address children’s health should also encompass limits for all restaurant menu items (Hobin 2014).
In 2011, the U.S. city of San Francisco put in place nutrient thresholds for chain restaurant meals marketed to children, including a limit of 640 mg of sodium per menu item (Otten 2014). While the restaurants did not change their menus directly in response to the policy, one chain restaurant did make side dishes and beverages more healthful, affecting the overall nutritional profile of orders.
Examples
Australia, Canada, New Zealand, UK and the USA: Hobin E, et al. Nutritional quality of food items on fast-food ‘kids’ menus’: comparisons across countries and companies. Public Health Nutr. 2014 Oct;17(10):2263-9.
San Francisco, USA: Otten JJ, et al. Impact of San Francisco’s toy ordinance on restaurants and children’s food purchases, 2011-2012. Prev Chronic Dis. 2014;11:E122.
Innovative/other policies for restaurants and street food
While there are many models for potentially reducing the sodium content of restaurant meals and increasing the number of lower-sodium menu choices for consumers, the following three approaches are innovative and promising, but have not yet been widely used or evaluated.
Marketing and pricing strategies
Possible marketing and pricing strategies include proportionate pricing (i.e., eliminating price discounts for large size products); pricing promotions for healthier menu items; and making fruit, salads, water, and other low-sodium items the default choice. Interventions that include how food is displayed and where it is situated on a menu or in a buffet can also affect consumer choices.
Food ordering websites and applications
Food ordering websites and applications can be used to promote lower sodium foods. For example, they can introduce prompts, warnings or suggestions to customers while they are placing an order to encourage healthier, lower sodium choices; they can suggest restaurants that offer low-sodium options; and they can rate restaurants according to the healthfulness of food options available.
Food safety infrastructure
For developing innovative approaches for the street vending environment, the use of food safety infrastructure may be particularly important. A street vendor model has been developed to optimize food safety and nutrition in South Africa, taking into account business viability. Surveys from food vendors in South Africa indicated high consumer willingness to purchase healthier items from street vendors and interest from vendors in organizing wholesale purchasing of healthier foods, both of which might support interventions to reduce sodium consumption (Hill 2019).
Examples
Singapore: Singapore Health Promotion Board. Healthier Dining Programme.
Thailand:
Thailand Sodium Lesstaurant program
New York City, USA: Angell SY, et al. Cholesterol control beyond the clinic: New York City’s trans fat restriction. Ann Intern Med. 2009 Jul 21;151(2):129-34. (Example of restricting artificial trans fat in restaurants, which may also be relevant to sodium)
Interventions for sodium added in the home
There are few effective programs to reduce dietary sodium in populations where the major source is sodium added at home. Most interventions to date have relied primarily on education; however, educational programs are often resource intensive and, on their own, unlikely to meaningfully reduce population sodium intake, especially after the conclusion of the program. Using a multicomponent approach may be necessary to meaningfully address sodium added in the home. The interventions listed in this section focus on scalable solutions that potentially have a larger reach.
Behavior change interventions
While also applicable to foods prepared outside the home or packaged foods, behavior change interventions are particularly important for salt added in the home; this is where people have the most control over their salt intake.
Successful interventions typically take a comprehensive approach. For example, in Vietnam (Do 2016), the Communication for Behavior Impact (COMBI) framework (Michie 2011) was implemented, which included mass media communication, interventions in primary schools, community communication programs, and targeted communications for high-risk groups, including people with hypertension. Post-intervention, follow up surveys found significant reductions in mean salt excretion (–1.99 g/day based on 24-hour urine samples) as well as significant improvements in knowledge and behavioral outcomes.
Other resources
Examples
Media campaigns *^
Media campaigns can motivate individuals to consume less salt by showcasing the dangers of a high-salt diet, demonstrating how to reduce salt intake (e.g., gradual reductions in salt or high salt condiments; using spices, herbs, and other flavors; checking food labels), and debunking myths related to salt consumption (e.g., rock salt or pink salt contains less sodium, people living in tropical areas need more salt, children need extra salt for growth/development, etc.). Key aspects of a successful campaign include:
- a clearly identified target audience
- key messages that motivate the target audience to reduce dietary sodium based on the major dietary sources
- a dissemination plan that fits the communications context, takes political context into account, and capitalizes on earned media
- an evaluation to assess the impact of the campaign.
Providing general nutrition information or recommendations to eat healthy foods have not been found to change behavior. When applying an existing campaign from another country, adapting the campaign to the local context is crucial.
In addition to encouraging behavior change, campaigns can be used to put pressure on government or industry stakeholders as part of the policy development process or to educate consumers about new policies to ensure successful implementation. For example, a mass media campaign was conducted in Chile to inform consumers about the meaning of the new front-of-package warning label policy and encourage them to choose products with fewer/no labels
Settings-based education
School-based education programmes have the potential to reduce salt consumption among children. Strong programs have created child-friendly icons and characters with positive, aspirational messages connected to healthy foods, and have encouraged children to act as change agents, bringing lessons home to their families. A randomized control trial of a school-based program in Northern China found a significant impact on sodium intake of the child and their family (He 2015).
Training can be provided to health care workers on the negative health impacts of high salt consumption and strategies for reducing salt consumption, and they can be encouraged to provide salt reduction counseling to their patients, particularly those with cardiovascular disease. For example, a salt reduction intervention in Fiji combined initiatives to engage food businesses to reduce salt in food with targeted consumer behavior change programs (through a health worker training program and public awareness campaign). The intervention resulted in a reduction in sodium intake from 11.7g/day to 10.3g/day (Pillay 2017).
Examples
Fiji: Pillay A et al. Assessment of a salt reduction intervention on adult population salt intake in Fiji. Nutrients. 2017 Dec 12;9(12):1350. (A broader behavior change program that included education through hospitals and health workers)
India:
Increase uptake of low-sodium salt^
Low-sodium salt typically replaces 10% to 50% of the sodium in regular salt with potassium (or in some cases, with magnesium and/or small amounts of other minerals). Interventions or policies to increase the uptake of low sodium salt should address:
- availability to ensure customers have access to low sodium salt by tackling production and regulatory challenges (e.g., access to potassium sources, infrastructure, and efficient supply chains)
- awareness and promotion (e.g., through education and social marketing campaigns) to ensure the public, shopkeepers, and health workers are aware of the product,
- affordability to equalize the price of low sodium salt and regular salt (sodium chloride) through use of subsidies, voucher programs, or by taxing regular salt (see Section 3.5 for more on fiscal policies)
- advocacy to ensure low sodium salt is on the governments agenda and garner support from salt industry.
Low sodium salt is one of the best strategies for reducing sodium in food made at home and can also be used in food manufacturing (or as part of implementing sodium targets (Section 3.3) and in restaurants or food services (Section 4.2).
It is important to note that while the added potassium in low-sodium salt can help combat potassium deficiency common in most populations and reduce high blood pressure, replacing more than 25-30% of sodium with potassium is often linked to a bitter or metallic taste. Further, there is some concern that potassium based low-sodium salt has potential for adverse effects due to hyperkalemia, specifically the increased risk of arrhythmias and sudden cardiac death, among individuals with medical conditions or on medications that impair their potassium excretion. While a few case reports of adverse events have been cited, there have been no reported excess risk of adverse events, including severe hyperkalemia, in studies evaluating the effect of low-sodium salts.
At the population level, overall health is improved with the use of low-sodium salt and risk is low. Given the limited potential risk, low-sodium salts can carry a warning to inform consumers of possible contraindications to low-sodium salt use that may increase risk for hyperkalemia ( JHU, RTSL 2021); however, these warning statements should not discourage consumers who have no contraindications.
Other resources
Examples
China:
Innovative/other policies to decrease use of sodium at home
Innovative or incompletely tested interventions are listed where evidence is still emerging or research on impact has been mixed.
Salt restriction spoons
Providing salt restriction spoons (usually holds 2g salt) along with instructions for adding salt to food may be helpful for sodium added at home or in small businesses (Chen 2013, Hou 2020).
Increased access to fresh fruits and vegetables
Natural foods have very little sodium. Many successful initiatives have improved access to fresh foods to reduce reliance on processed foods high in sodium often used in home cooking. Removing barriers such as price and low availability can help to increase access to fresh foods (E.g., FAO PAA). See Section 3.5 for more on subsidizing healthy food like fruits and vegetables.
Interventions on popular foods preserved in salt
In many regions, meat, fish and vegetables preserved in salt or stored in brine are popular and may even be required for food preservation where refrigeration is not easily accessible.These foods can be store bought or pickled/preserved in the home depending on the country or context. Rinsing, washing or soaking the food in water before cooking or serving can reduce the salt content. More research is needed to determine the most effective methods of reducing salt content while preserving other nutrients and preventing pathogen growth. In Korea, a special refrigerator was developed to allow storage of lower sodium Kimchi.
Sodium warning labels
Salt containers can be required to carry a warning label on the front of the package (Campbell 2019). Argentina has developed a regulation requiring that packages carry the warning: Too much sodium in the diet causes high blood pressure and increases risk of stomach cancer, stroke, heart disease and kidney disease. Limit your use.
Appendices and Acknowledgements
Appendix 1. Sodium reduction program checklist
The following Excel file provides an interactive checklist that summarizes each step within the Sodium Reduction Framework. It can be used to track and monitor the status and progress of current sodium reduction programs, identify gaps in national strategies, and provide direction for prioritization in future programs and strategies.
Appendix 2. Example content of a situational analysis for preparing a sodium reduction strategy
The WHO describes a situational analysis as “an assessment of the current health situation…fundamental to designing and updating national policies, strategies and plans.”[1]
An in-depth description of how to conduct a situational analysis for a national health policy is described in the WHO Situation Analysis in the Health Sector and includes a list of the stakeholders who should be involved, key characteristics of the analysis, links to tools for conducting an analysis, and a sample outline of a report. A participatory approach, which includes making information available to citizens and representatives from sectors that intersect with health, can enhance transparency and accountability. The analysis should assess not only the context for reducing population sodium intake, but the underlying causes, such as the social determinants of health, that have contributed to high sodium intake. It can also include a description of stakeholder roles and responsibilities, to understand which organizations hold formal and informal power.
The situational analysis may include answering the following types of questions to assess the strengths, weaknesses, opportunities, and threats to creating a national sodium reduction strategy:
Political support and opposition:
- What level of support and opposition to reducing dietary sodium exists at multiple levels (political, food industry, general public, health and scientific community) and how is this support expected to change over time?
- What are the expected economic and health advantages of a sodium reduction program?
- Are current policies to minimize financial conflicts of interest adequate?
- Is there likely to be organized opposition from individual companies, food industry groups or other organizations?
- Are there strong platforms to monitor food and salt industry influence (e.g., consumer protection groups)?
Monitoring and Evaluation:
- What data has already been collected on sodium intake, sources, or content in foods?
- How do levels of sodium intake and sources of sodium vary by geography, age, ethnicity, gender, or for other subgroups?
- What surveys, research and laboratory services are available to estimate overall sodium intake, the major dietary sources of sodium and the sodium levels of key foods and what steps need to be taken to fill any gaps?
- What is the perception of the general public on the main sources of sodium in the diet, the health impact of consuming too much sodium, and the importance of reducing sodium intake?
Strategy:
- What financial and other resources are available or likely to be obtained?
- What are the program needs that can be filled by key stakeholders and collaborators (e.g., education and advocacy, research, monitoring and evaluation, technical skills without conflicts of interest in reducing sodium content of foods)? This should include a stakeholder mapping exercise.
- What healthy food policies are already in place/planned; do they or can they integrate sodium reduction directly (e.g., sodium targets for foods) or indirectly (e.g., healthy public food procurement)?
- What regional and international legal frameworks could help/hinder the promotion and implementation of sodium reduction policies?
- Are there any current communication campaigns, by public health agencies or food companies, about nutrition and health or sodium intake specifically?
- How can critical groups, such as the household food purchaser/preparer, and vulnerable groups (e.g., ethnic minorities, low literacy adults) be reached?
- Where does the general public get health/nutrition advice from?
[1] World Health Organization. Situation analysis and priority setting, 2018.
Appendix 3. Instructions for developing a food database
INSTRUCTIONS FOR DEVELOPING A PACKAGED FOOD DATABASE THROUGH A SHOP SURVEY
Guidance on conducting a shop survey: Instructions for steps 1-7
| Step 1 |
Determine the food categories and stores where information will be collected from The objective here is to collect data on the main foods that contribute to salt in the diet from a range of stores (small shops and supermarkets). The main contributors to salt in the diet can be identified from dietary surveys; however, in most countries key contributors to salt from processed foods are likely to be bread and other baked goods, processed meats and cheeses, canned or salted fish, noodles, crisps and snacks, and sauces and condiments. Sodium content data for all product categories should be collected to ensure the most complete dataset. Products within the same categories should be collected regularly (e.g., annually) to monitor changes in product formulation as well as new product development. The process can be made more efficient by regulating the standardized disclosure of nutrient content of packaged foods. This may include requiring manufacturers to post nutrition information online or creating a surveillance plan to audit products during routine store visits by the Ministry of Health. For most countries, the collection of data should include all nutrients of concern (e.g., sodium, sugars, saturated fats) as well as calories to allow nutrients to be expressed per kcal as well as per 100g. |
||||||||||||||||||||||
| Step 2 |
Set up research team and prepare data collection materials The size of the research team will depend on the number of processed food products on the market and the need to audit products in stores vs. searching in online databases or receiving standardized information from stores or food processors. For in-store audits, many countries will need a project coordinator and a team of 4-5 people to collect data over a few weeks (generally, a team of two can manually collect/photograph 40 products per hour). Once the team has been established, materials to collect data need to be prepared. Collecting data with a tablet or a smartphone is preferred, but copies of the record sheets can be printed out for manual recording if necessary. Photographs should be taken of each side of the product label, including the Nutrition Facts Label (NFL). The project coordinator should assign each person one or two product categories and all information for all products within the category should be entered. |
||||||||||||||||||||||
| Step 3 |
Gain permission from store owners to collect data Before data can be collected in stores, seek permission from store owners. Usually, it is sufficient to go and introduce yourself and explain what you are doing when you get to the shop but in some cases, it may be necessary to send a letter first and then follow up with a visit to request permission prior to conducting the survey. |
||||||||||||||||||||||
| Step 4 |
Conduct surveys (recording information from the packaged food labels) Option 1: Manual data collection The research team will record information from all food items using a data collection template. Each product should be given a number. Even if the sodium data is missing from a product, the other product details should be recorded. If a product is not labelled or the label is in a different language this should also be recorded so that it will be possible to calculate the percentage of products without labels or that are incorrectly labelled. Photographs of product labels and NFLs is helpful for documentation and data verification. Sometimes, only photographs are taken during the actual in-store visit, and data from the photographs is entered into the template at a later date. Step 4a – Find the Nutrition Facts Label
Step 4b – Find the information for ALL of the criteria in the table below
Step 4c – Copy the information from the nutrition information panel into the data collection template Option 2: Using a smartphone data collector application An alternative to collecting the data manually is to use a smartphone-based application, such as the George Institute for Global Health’s FoodSwitch mobile App, the Food Label Information Program (FLIP) App from the University of Toronto, and the NutrINSPector App developed by the National Institute of Public Health of Mexico (INSP). Generally, these applications assist countries in collecting information about the nutritional composition of processed foods in the supermarket. The apps can be used to take photos of the front of the package, the Nutrition Facts Label (if present), the ingredient list, and scan barcodes if they exist on the package. Photos can be uploaded to a cloud storage server. Photos are viewed there or downloaded to enable a research team to enter the nutrition information for each packaged food item. |
||||||||||||||||||||||
| Step 5 |
If data was collected manually, enter the information from the data collection template into a database (organised by food category) Manually collected data needs to be entered into a standardised database, often Microsoft Excel, Access, or REDCap. Each item also needs to be put into a relevant food category to ensure that information can be analysed in a systematic way. The categorisation of foods may differ between countries to some extent. However, countries may choose to use broad categorisation systems developed by the WHO or regions (e.g., PAHO) that should enable cross-country comparisons. |
||||||||||||||||||||||
| Step 6 |
Do quality checks of the database: screen for plausibility and check 5-10% of products against original source The data entry process needs to be verified. A random sample of 5-10% of entries should be selected and the information in the database should be compared against the online records, original in-store audit record sheets, photographs of product NFLs, and if necessary, against the original products in stores. It is important to note that the NFL may not accurately reflect the sodium content of the food. Having a separate process to verify the actual sodium content (through independent chemical analysis of the products) to compare to the NFL is optimal. |
||||||||||||||||||||||
| Step 7 |
Conduct data analyses to determine the mean levels of nutrients in each food category (at minimum) There should be an initial tabulation that summarises the number of products in each food group and each food category. Mean and median levels (and ranges) for sodium should be calculated overall and, if possible, separately for the leading companies contributing to each food category. The primary analyses should be reported per 100g, but additional estimates can be made per serving if this is relevant. The gold standard is to assess the sales weighted average for sodium in a category; however, most countries do not currently have ready access to sales weighted data. |
Information about Global Food Monitoring Group
This resource is adapted from the Global Food Monitoring Group. The health problems caused by processed foods are global and the Global Food Monitoring Group has initiated an international effort to track the nature of processed foods around the world. The ‘Food Monitoring Group’ includes representatives from ~30 developed and developing countries who have developed a protocol for tracking the nutritional composition of processed foods. Low cost, readily available data collection and management tools have been developed and provide a sustainable low-cost mechanism for acquiring data on the nutritional composition of foods at scale. The data will in turn allow monitoring the effectiveness of global efforts to ameliorate ill health caused by processed foods and hold governments and corporations to account for the quality of the products that are marketed. For more information about the Global Food Monitoring Group or using the Data Collector App see: http://www.georgeinstitute.org.au/projects/global-….
Acknowledgements
This document was developed by Resolve to Save Lives: Dr. Laura Cobb, Nicole Ide, Funke Ajenikoko, Kate Elliott, and Dr. Jennifer Cohn and RTSL consultants: Dr. Norm Campbell and Christine Johnson . The document was also reviewed by the following individuals:
Dr. Renu Garg, Medical Officer – WHO Country Office Thailand
Dr. Sushera Bunluesin, National Professional Officer – WHO Country Office Thailand
Payao Phonsuk, Food and Nutrition Policy for Health Promotion Program, International Health Policy Program Foundation, Thailand
Dr. Champika Wickramasinghe, Ministry of Health, Colombo, Sri Lanka
Dr. Renuka Jayatissa, Medical Research Institute, Ministry of Health, Colombo, Sri Lanka
Dr. Nalika Gunawardena, National Professional Officer (Noncommunicable Diseases and Health Systems) – World Health Organization, Sri Lanka
Dr. Karen Charlton, School of Medicine and Illawarra Health and Medical Research Institute, University of Wollongong, New South Wales, Australia
Dr. Feng J He, Wolfson Institute of Preventive Medicine, Barts and The London School of Medicine & Dentistry, Queen Mary University of London, United Kingdom
Dr. Eduardo Nilson, Center for Epidemiologic Research on Nutrition and Health, University of Sao Paulo, Brazil
Adriana Blanco-Metzler, Researcher – Costa Rican Institute of Research and Teaching in Nutrition and Health, Costa Rica
Dr. Jacqui Webster, The George Institute for Global Health, University of New South Wales, Australia
Leo Nederveen, Advisor Food, Nutrition and Physical Activity in Schools – WHO Regional Office for the Americas, Pan-American Health Organization
Lorena Allemandi, Consultant – WHO Regional Office for the Americas, Pan-American Health Organization
Azeb Tolessa, Senior Program Manager, Nutrition – Resolve to Save Lives, Vital Strategies
Dr. Zeng Ge, Chief Technical Officer, Sodium Reduction and Surveillance – Resolve to Save Lives, Vital Strategies
Dr. Maryam Al-Mansur, Nutrition Policy Advisor – Resolve to Save Lives, Vital Strategies
Dr. Meenu Singh, Technical Advisor-Nutrition – Resolve to Save Lives, Vital Strategies
Dr. Swati Bhardwaj, Technical Advisor: Nutrition – Resolve to Save Lives, Vital Strategies
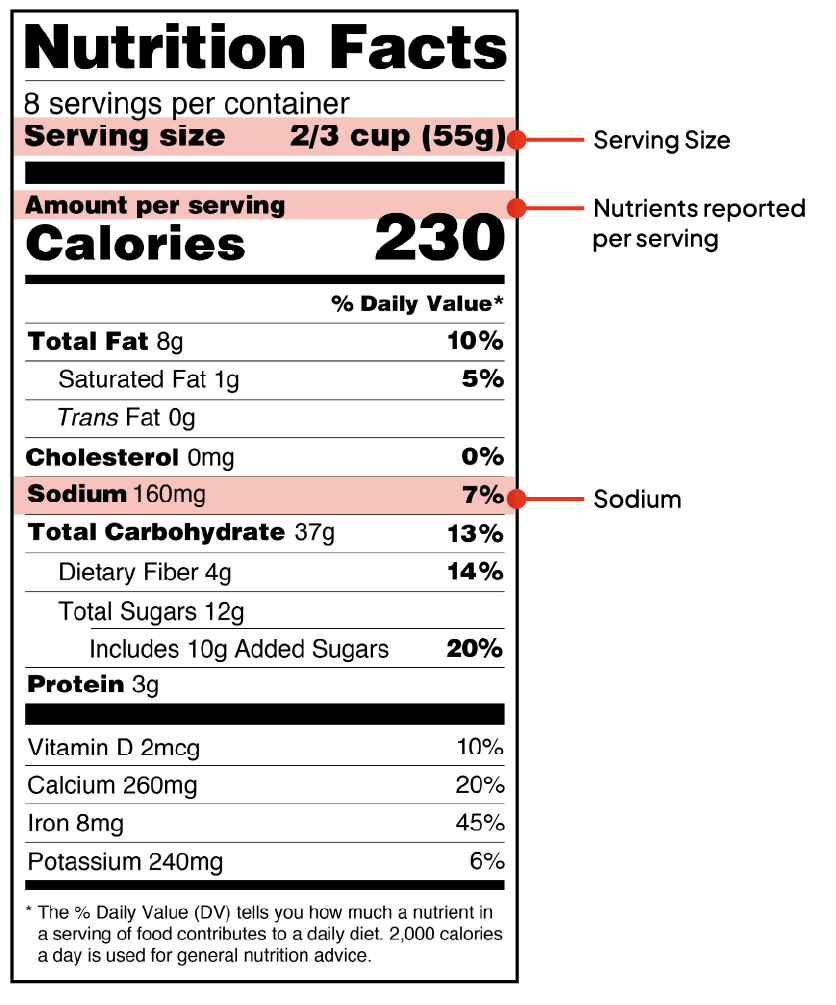
Social marketing
Social marketing applies commercial marketing principles to influence social behaviors. A strong social marketing framework will 1) identify one segment of the public whose behavior it hopes to influence, 2) ascertain what drives people to consume high salt products, 3) isolate a single, immediate benefit that will make it worthwhile to give up high-sodium products, 4) focus on one behavior to change at a time, facilitating the desired behavior and evaluating the outcome, and 5) deploy surprising messages to catalyze behavior change (Khalig 2019).
One use of social marketing campaigns is to promote and increase uptake of low sodium products, such as low sodium salt or condiments. Ideally, the campaign would promote the product (low sodium salt or other low sodium food), while considering both the price (cost and access) and place (retail settings). For example, a research study in Peru facilitated the uptake of low sodium salt using social marketing principles, which led to a reduction in blood pressure and an increase in potassium intake (Bernabe-Ortiz, 2020).
Other resources
Pan American Health Organization. Introduction to social marketing for public health. 2020. (Online course)
Pan American Health Organization. Applying a Social Marketing Framework to Salt Reduction. 2012.
Khalig M et al. Salt reduction in Latin America: A Regional Social Marketing & Communication Plan. Project – IDRC 108167 Scaling Up and Evaluating Salt Reduction Policies and Programs in Latin American Countries. 2016-2020 Tres Ríos, Costa Rica: Costa Rican Institute of Research and Teaching in Health and Nutrition (INCIENSA), 2019.