The challenge
Of the roughly 4.3 million people suffering from high blood pressure in Sri Lanka, only 16 percent have it under control, putting them at risk of heart attack, stroke, and premature death.
The solution
Resolve to Save Lives partnered with Sri Lanka’s Ministry of Health to pilot a quality improvement (QI) program that leveraged real-time data on a custom dashboard. Program managers used the new QI program to identify treatment inertia as a bottleneck and implemented measures to address it.
The impact
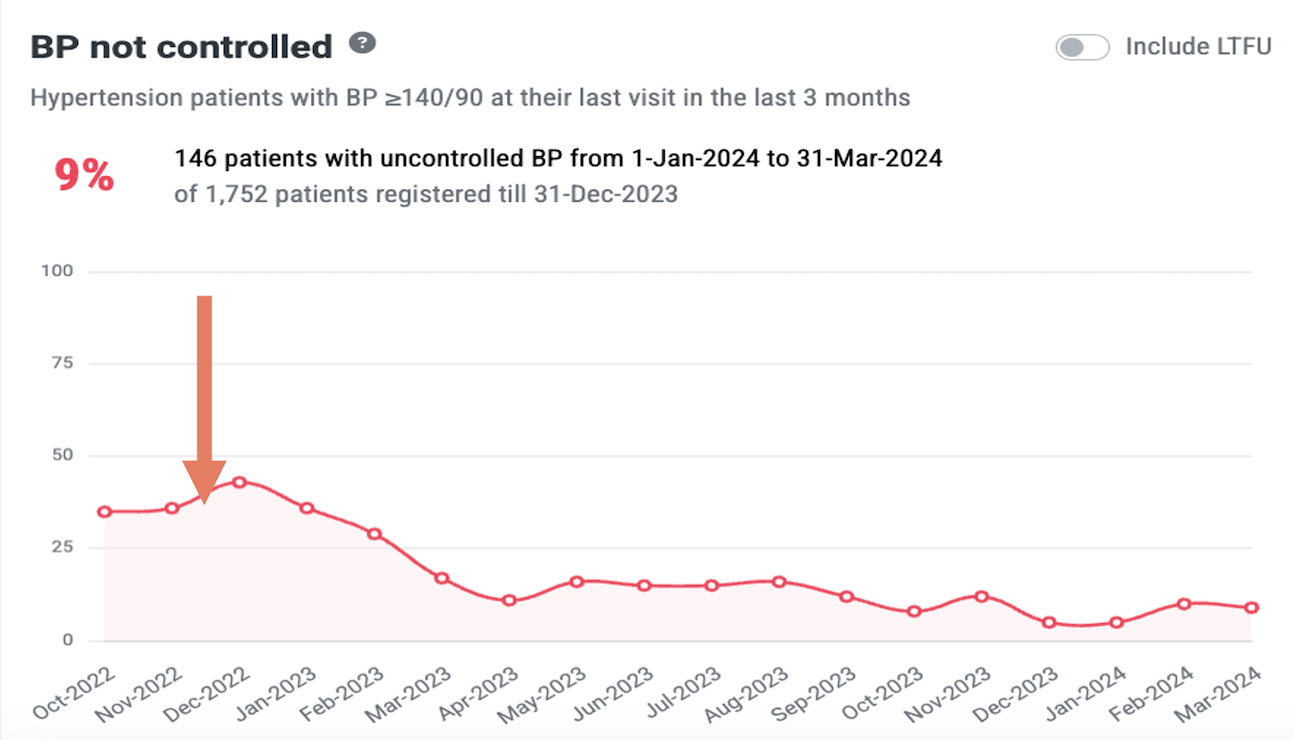
Over the course of a single year, medication titration increased by over 50%, playing a key role in raising blood pressure control rates from 50% to 68%.
The challenge
How do we help millions of Sri Lankans get their blood pressure under control?
Recognizing the need to tackle high blood pressure at scale, the Sri Lanka Ministry of Health (MoH) adopted the WHO HEARTS technical package for hypertension control in 2021.
The ultimate goal of a successful hypertension program is to control blood pressure. Diagnosing is important to find those at risk, and initiating treatment is a crucial first step. But it is through controlling high blood pressure that programs help reduce their patients’ risks of a disabling event and improve outcomes. With the HEARTS program in place, Sri Lanka needed to next determine if their hypertension control program was in fact controlling high blood pressure, and to quickly implement interventions to address the reasons if it wasn’t.
The solution

Resolve to Save Lives’ quality improvement approach
With technical support from RTSL, Sri Lanka’s MoH implemented a quality improvement package in three pilot facilities in December of 2022.
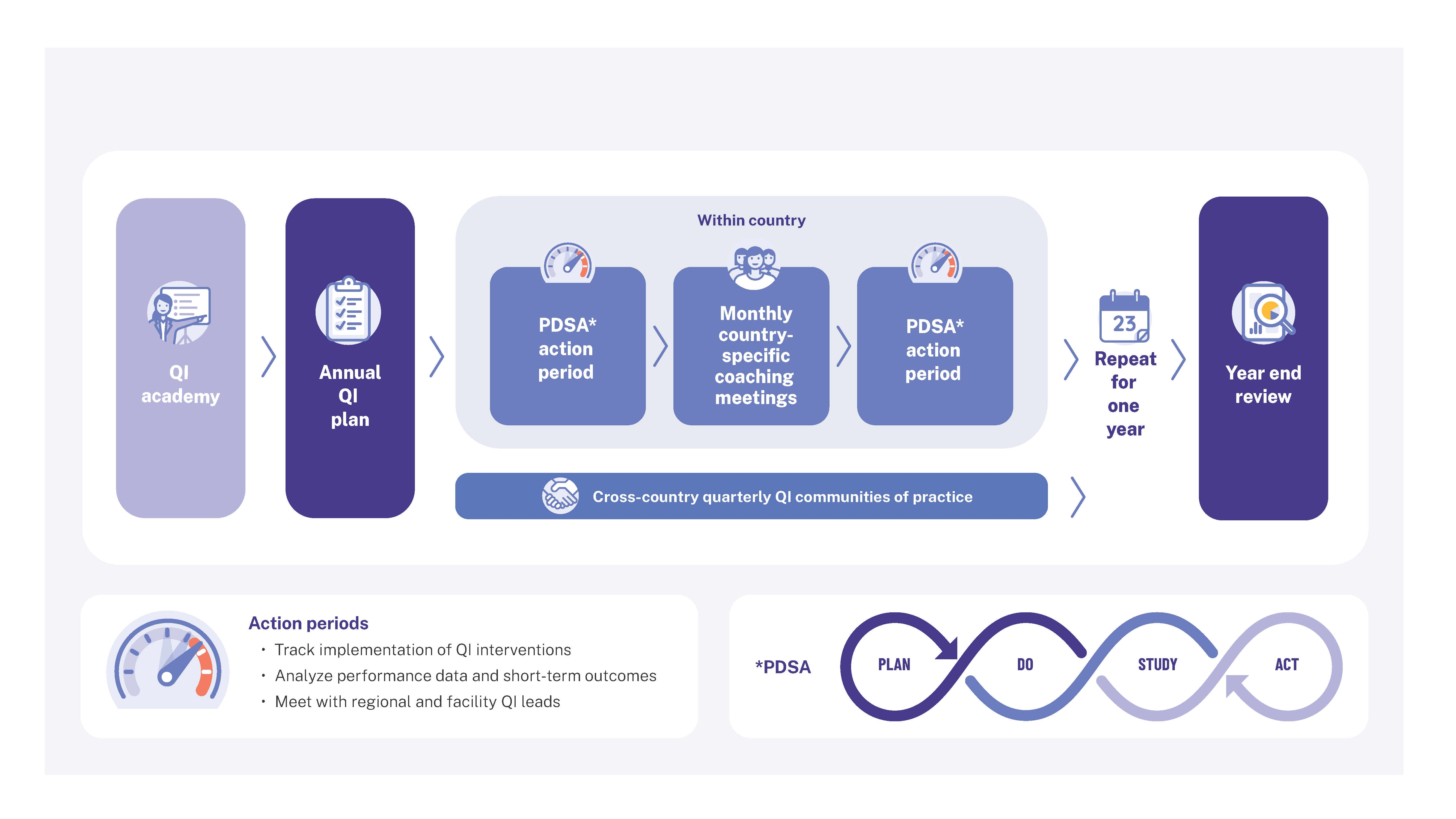
Quality improvement is an approach that uses regular assessment of program data to identify gaps between actual outcomes and desired outcomes, and determine what factors are responsible. Program managers then create interventions to address those gaps. Continued monitoring and assessment determine if the interventions are working and worthy of scaling—creating a virtuous cycle of feedback.
Sri Lanka’s QI program included three main components:
- QI training for program managers;
- A simple digital dashboard for monitoring; and
- Monthly QI meetings to evaluate and iterate interventions.
QI training for program managers
National hypertension program managers attended RTSL’s Quality Improvement Academy, which focused on how to analyze data, identify gaps in care, test targeted interventions, and conduct monthly quality improvement meetings to assess progress. The Academy included 23 national hypertension quality leaders from eight countries and involved multiple virtual trainings over the course of 3 months facilitated by Resolve to Save Lives.
At the end of the training, each country developed an annual plan with interventions to target the main drivers of BP control:
- Drug supply
- Missed patient visits
- Decentralizing care
- Medication titration
A simple digital dashboard for decision-making
Program managers used the HEARTS360 dashboard, which is pre-configured with WHO HEARTS indicators for hypertension and diabetes and enables rapid performance assessments and real-time comparisons across facilities. Data in the dashboard is updated daily in settings with a digital information system such as Simple or DHIS2. In Sri Lanka, health care workers input just a handful of key indicators into the Simple app so program managers can use the resulting dashboard to assess the progress of their interventions and inform next steps.
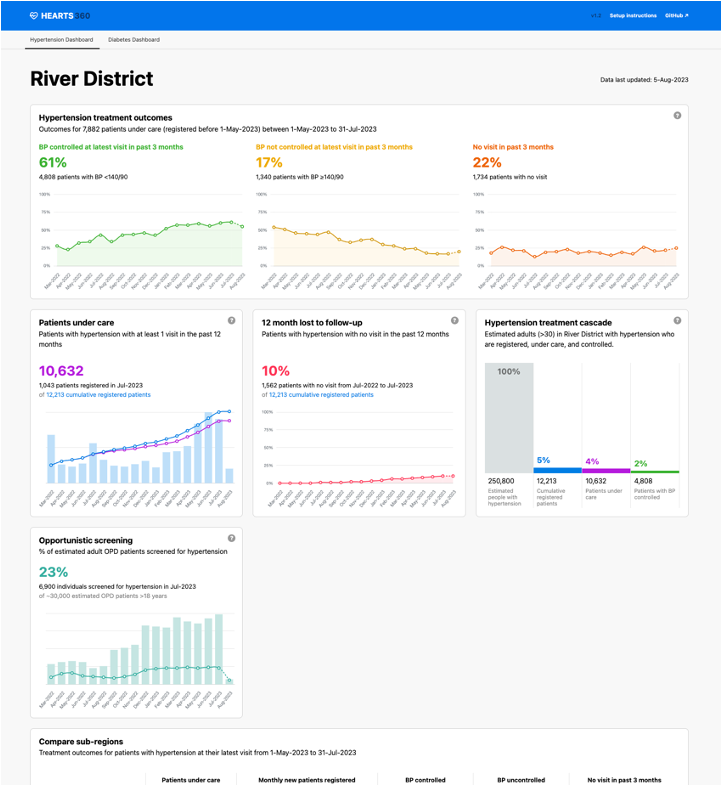
Iterative interventions
Monthly and quarterly QI meetings to assess progress of interventions were pivotal to improve program quality. Monthly meetings consisted of a national quality leaders trained by the academy and RTSL quality improvement experts who reviewed reports produced by the HEARTS360 dashboard to determine next steps across the national program. Quarterly, the Ministry of Health NCD Unit leaders met with district officials and facility champions to review the data and share learnings and best practices, encouraging improvement and structuring accountability.
The impact
Finding—and reducing—treatment inertia
The QI program revealed a major bottleneck to blood pressure control: some patients were returning to the facility for a follow up with their blood pressure uncontrolled; in many cases, instead of intensifying their treatment, clinicians were maintaining them on the same drug and dose they had before. This challenge, known as treatment inertia, is not unique to Sri Lanka—globally, clinicians in low- and middle-income countries adjust medications in such cases less than 20% of the time. But it can undermine the effectiveness of a hypertension control program.
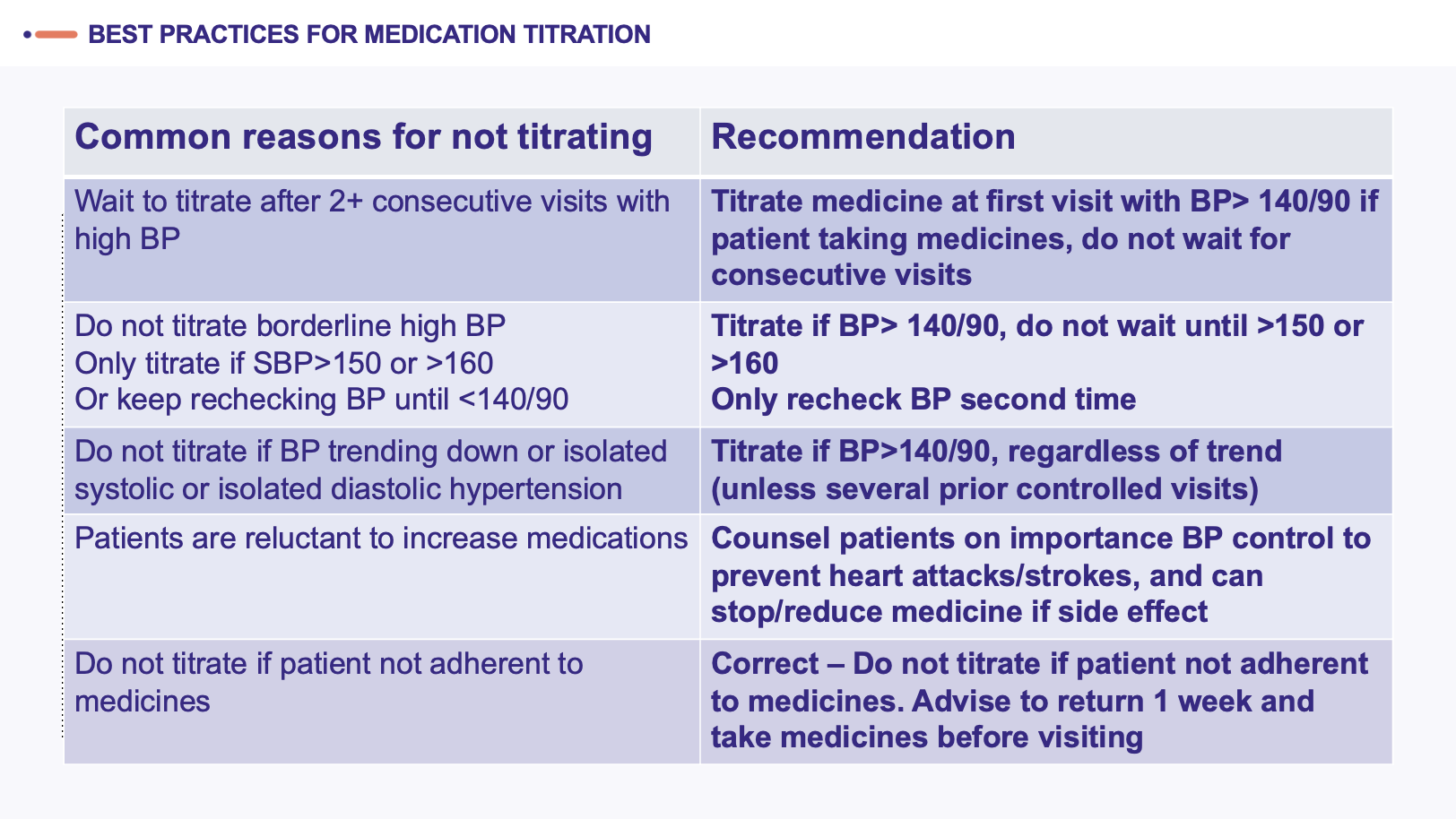
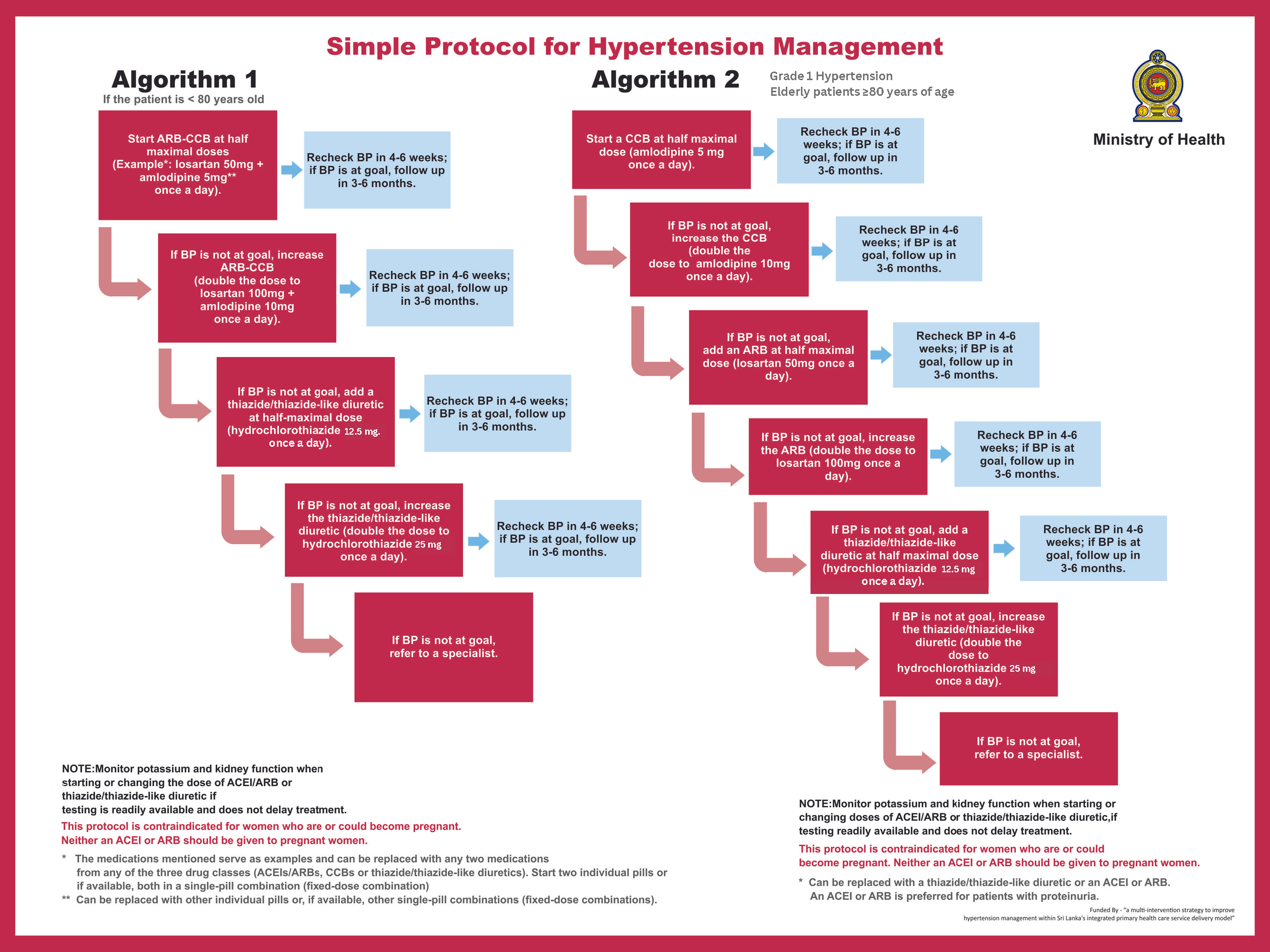
The pilot facilities implemented a comprehensive package of quality improvement interventions aimed at addressing the causes of treatment inertia. A local clinician who championed this effort, Dr. Amila of the DH Haltota pilot facility, conducted clinician trainings that focused on best practices for titration. They also worked with the MoH to reinforce use of the national simplified treatment protocol with just a few key medications and clear titration guidelines. Streamlining prescription processes not only standardized care but also reduced medication costs and increased availability by enabling bulk procurement. Quarterly reviews of medication titration data highlighted best practices that were shared amongst the clinicians, while reminders from health care workers encouraged patients to take their medications consistently and refresher trainings ensured health care uploaded data into the digital tool correctly.
The evidence is clear – lower blood pressure is better. But we see that clinicians are often reluctant to increase medications until blood pressure is controlled, and that can undermine the impact of a hypertension control program. Using a quality improvement approach and local clinical champions, we were able to identify the barrier and train clinicians on the importance of following a simple treatment protocol. And it worked.
Dr. Reena Gupta, Chief Medical Officer for Performance Improvement, Resolve to Save Lives, Professor of Medicine, Univsersity of California, San Francisco
The interventions worked. Within just one year of routine quality improvement meetings and an iterative intervention and assessment process, medication titrations according to protocol in the three pilot facilities increased by more than 50%. This contributed to a cross-facility increase in blood pressure control from 50% to 68%
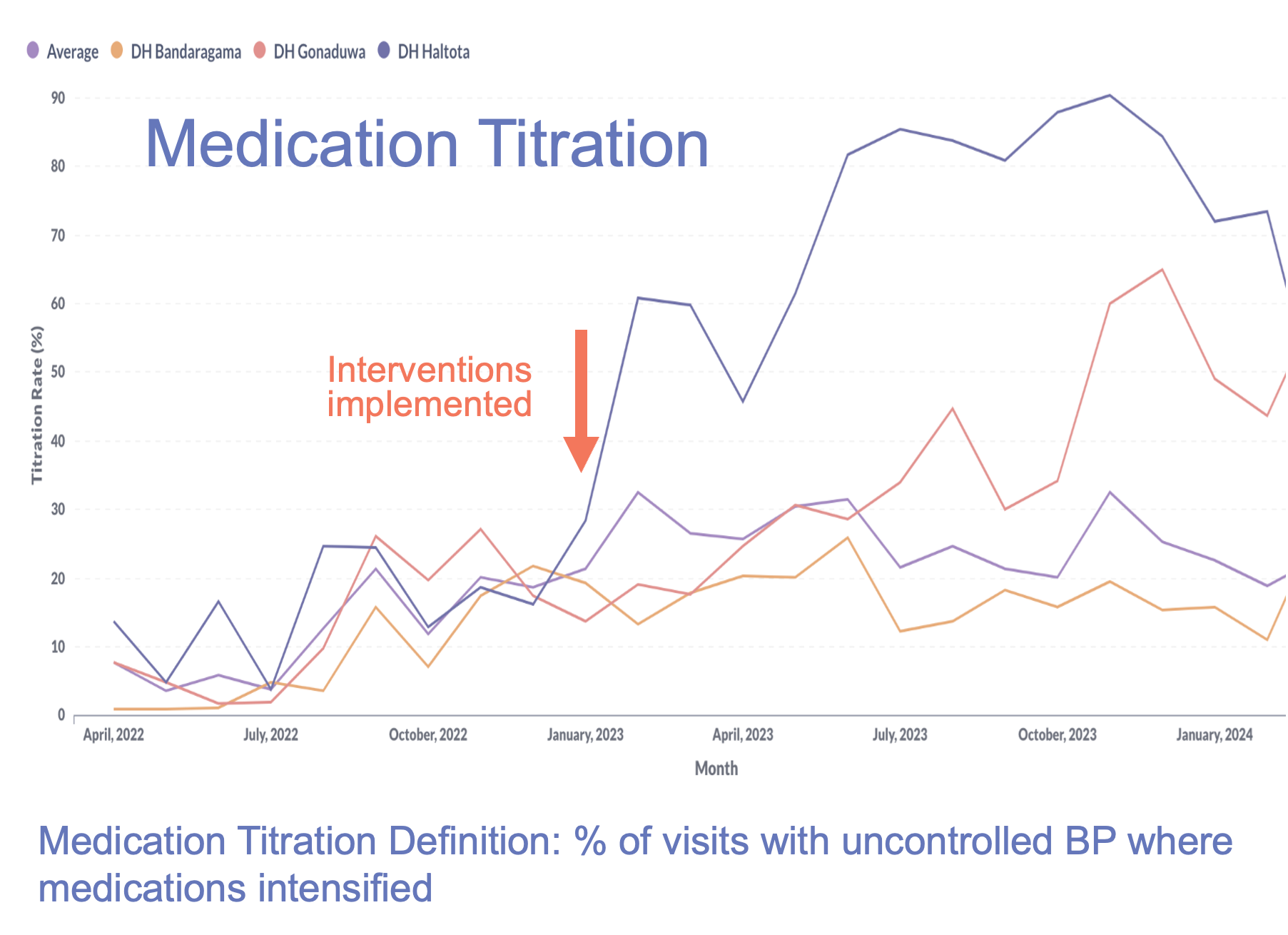
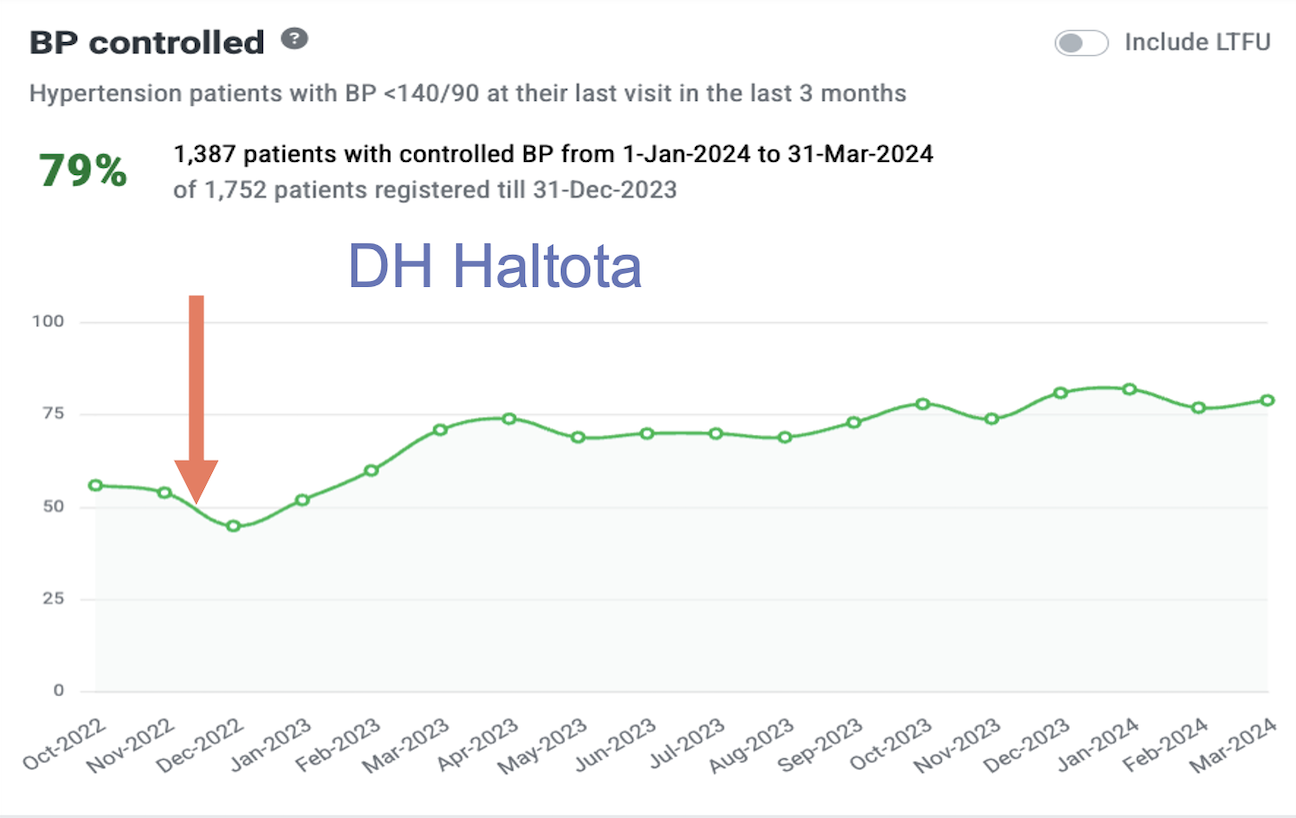
Due to the success of these pilot facilities, the Sri Lanka MoH added the QI interventions for medication titration to 11 hospitals in January 2023 and 10 more hospitals in December of 2023. Sri Lanka MoH has also committed to scaling the QI program to all project facilities throughout the country over the coming years. Sri Lanka’s journey demonstrates how leveraging data, fostering accountability, and standardizing care can transform hypertension control programs, saving lives and strengthening health systems for the future.
Blood pressure control is key to reducing health risks from hypertension, such as heart attack and stroke. After implementing the WHO HEARTS technical package, we needed to verify if our interventions were working and where we could improve. The QI Academy gave us the tools we needed to adapt our approach until we found what works. In our continued commitment to improving the lives of all In Sri Lanka, we have plans to expand these interventions and to continue using the QI approach.
Dr Champika Wickramasinghe, Deputy Director General (NCD), Ministry of Health, Sri Lanka



